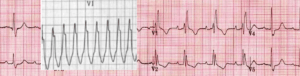
Here is a simple case of potential ventricular tachycardia(VT) How do you manage this?
A patient has been brought into your resuscitation cubicle with the a complaint of palpitations. His ECG is as follows:
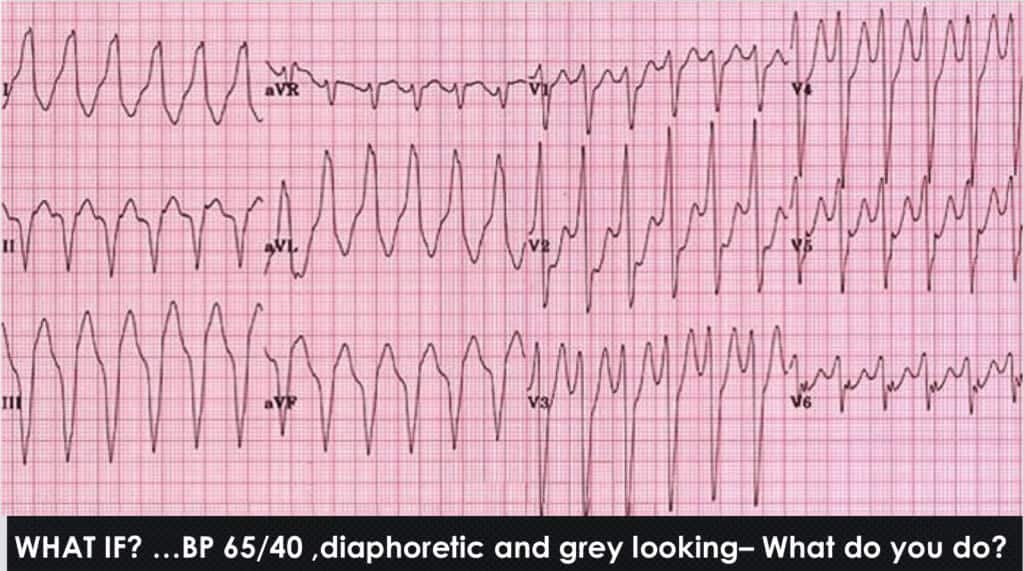 The patient is obviously unstable, so the management decision is easy: ELECTRICITY.
The patient is obviously unstable, so the management decision is easy: ELECTRICITY.
What if the patient is stable with a BP of 138/65 and is sitting up in bed texting on their phone. Many would argue for the same treatment. However, the fact that they are stable does mess with our minds, just a little. We become unsure. We may subconsciously weigh up the risks of sedation and delivering electricity to giving a drug. It sets up a degree of uncertainty.

Here is an example:
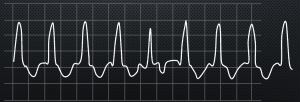
A 19 yo woman presents with palpitations and feeling unwell. She has no past history. Her vitals are stable including a BP of 125/60. Her ECG is shown below:
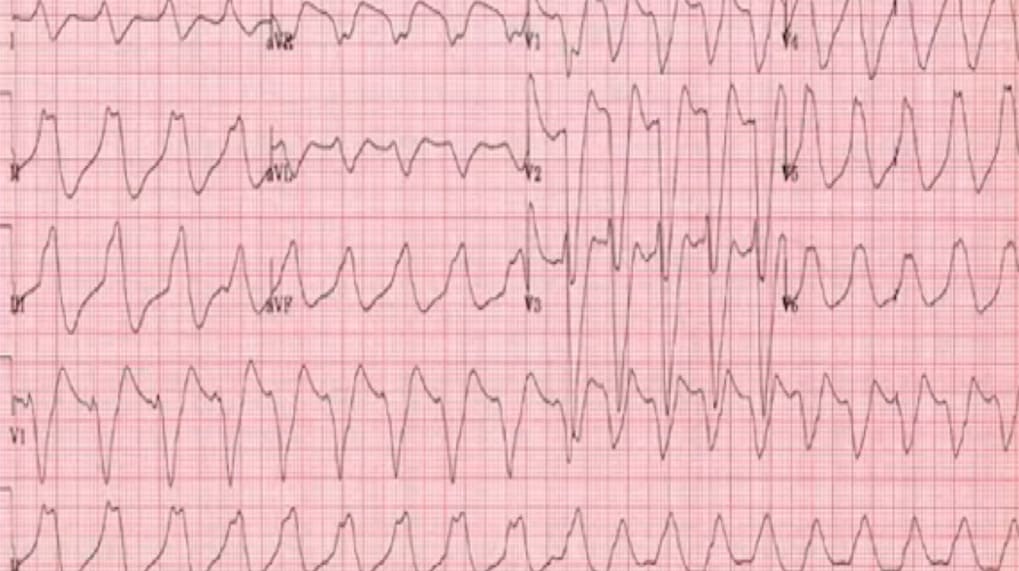
As she is stable, she is treated with IV Amiodarone and proceeds to have a bradycardia arrest and cannot be resuscitated. Why? because this isn’t VT. It’s hyperkalemia. The patient had a K of 9.3 mmol/L
Sometimes we should just sit back and think and watch rather than do.

Caused of Wide Complex Tachycardia(WCT)
- Ventricular Tachycardia (VT)- 80% of cases are VT
- SVT with aberrancy
- Hyperkalaemia
- Na Channel Blockade
- Paced Rhythm
How to Diagnose VT
There are multiple rules that can be used:
- Brugada Criteria: Rule in VT. Sensitivity 92%, Specificity 65%
- Vereckei Criteria: Rules in VT: Similar Sensitivity and specificity to Brugada
- Griffith Criteria: Rules in SVT. Sensitivity 90% Specificity 75%
The problem with these rules is that they are not sensitive enough and they lack consistency across observers. If you sit a group of cardiologists down and ask them to apply them, they will disagree.
My 5 rules for diagnosing VT
-
Is it faster than 120 beats per minute?
- For monomorphic VT, the rate must be greater than 120 beats per minute in order for the diagnosis of VT to be made.
- The example above of the 19 yo with WCT, who had a bradycardia arrest post amiodarone, demonstrates a rate of 114 beats per minute. It was not VT.
-
Is it wider than 120ms?
- This is based on the Brugada algorithm which confirms VT if RS> 100ms. I make it easier by looking at the QRS and asking if it wider than 3 small squares.
- Of course beware of the bundle branch block characteristics
- Beware also of the very wide complexes. Bizarre wide complexes should make us think of Hyperkalaemia
-
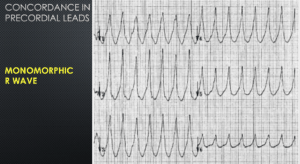
Is there Concordance?
- This really asks if all the precordial leads have either a monophonic R or S wave
- A simpler way of saying this is, do all the precordial leads predominantly point in one direction?


-
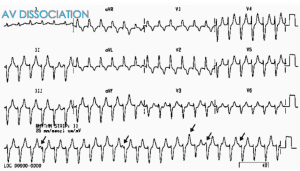
Is there AV Dissociation?

-
Is there a characteristic morphology?
- Are there Capture Beats or Fusion Beats?
- Capture Beats are narrow beats, that represent normal complexes. They confirm VT

- Fusion Beats occur when the beat from the AV Node fuses with the beat from the ventricles, resulting in an intermediate-looking beat

- Capture Beats are narrow beats, that represent normal complexes. They confirm VT
- Is there a Right Bundle Branch Morphology in V1?
- Look for the Rsr pattern ie., the right rabbit’s ear being up.

- Look for the Rsr pattern ie., the right rabbit’s ear being up.
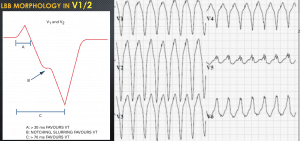
- Is there a Left Bundle Branch Morphology in V1/2?
- Look for the notching of the S wave, also known as Josephson’s Sign. It confirms VT
- The distance from the QRS onset to the nadir of the S wave being >100ms. It confirms VT.

- Is there a QR in V6?
- This applies to either RBBB or LBBB patterns

- This applies to either RBBB or LBBB patterns
- Are there Capture Beats or Fusion Beats?
Below is the Video of my Lecture from this year’s Cardiac Bootcamp.
This video and many others can be viewed by purchasing a subscription to EMCORE Digital.
Peter Kas