Tranexamic Acid: Did we find another Use?
So, picture a case. A 45 year old man presents to your Ed with spontaneous tongue, lip and face swelling. His only medical history is hypertension, for which he takes perindopril….
I could give you a lot more diagnostic information – vital signs, symptoms etc to facilitate you to exclude trauma, anaphylaxis and sepsis as a source of his presentation, but let’s cut to the chase and get to the bit I want to talk about…. this is similar to a case we had in the other day, and a colleague proposed trying tranexamic acid. If you’re confused now, you’re about exactly where I was! We had a patient with a likely diagnosis of ACE induced angioedema. I could see my way to some crazy stuff like Icatibant, but my generally better-read colleague pointed out to me there was a small amount of evidence for tranexamic acid in this situation.
Let’s step back.
We’ve discussed tranexamic acid at EMCORE before. Peter asked me to come up with 101 uses for it and present. Sadly, I was a trifle short of the requisite number.
Even with the help of the extended faculty, (including *extremely* helpful suggestions such as using it to cut heroin, or for treating pets’ facial cancers) we were able to come up with a reasonable list of uses.
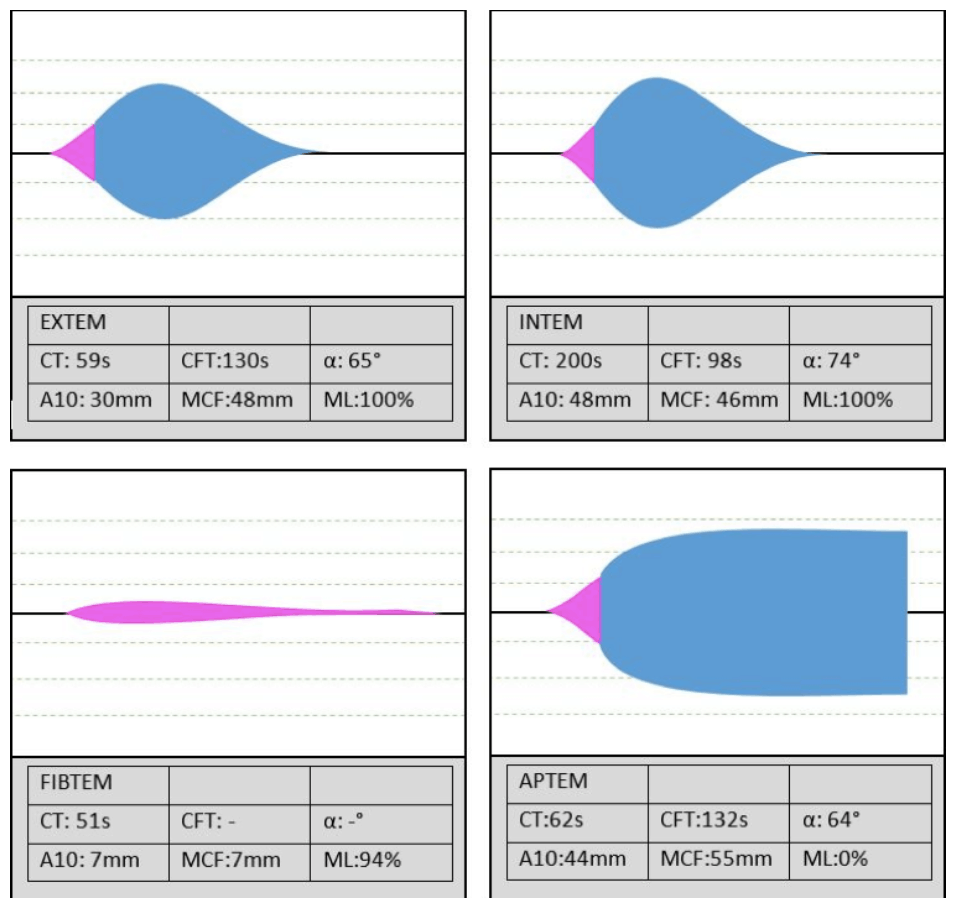
Of course CRASH-2 showed TXA’s empiric utility in trauma. That’s old news. My personal view is that now that thromboelastography can determine whether a sample of blood is subject to hyperfibrinolysis or not (image below[1]) there will be a lessening off the overall empiric user of TXA for major bleeding.
The same story goes for post-partum haemorrhage (WOMAN showed a decrease in death due to exsanguination), and I suspect will also be the same for GI bleeding, nothing that the results of the HALT-IT trial are still to be published.
In short there probably is a role for empiric TXA in the setting of major bleeding if patients cannot be specifically selected by rotem analysis.
Tranexamic acid is also useful topically:
- A cotton pad soaked in 10% TXA stops 73% of nosebleeds in 10 minutes, compared to 29% with conventional packing. There is also less rebleeding at 1 week (5% v 21%).[1]
- Gauze soaked in 4.8% TXA is 1.6 times more likely to arrest bleeding from dental extraction sites compared to normal packing.[1]
- Nebulised TXA 500mg doubles the rate of cessation of haemoptysis at 5 days compared with saline (95% v 50%).[2]
But what about angiooedema?
At the heart of the desire to treat with TXA is a small retrospective study from 2014[3], looking at prevention of attacks of hereditary angiooedema with prophylactic administration of txa. There were 35 patients enrolled in the cohort. With the administration of tranexamic acid, half the patients experienced a 75% reduction in the frequency of attacks. A further ten patients experienced a reduction in the severity of attacks. No patients experienced an increase in the severity or frequency of attacks.
It’s a long way from prophylaxis of hereditary angiooedema to the score treatment of idiopathic ACE induced angiooedema, but on the other hand if you stick the patients from CRASH-2 and WOMAN into a gigantic pile, there’s 40000 pieces of randomisation that say tranexamic acid is a safe drug to give (which incidentally is one of the most underreported and in my mind significant findings of these studies…). So, what did we have to lose?
Nothing.
Did it help? Unfortunately not – our patient still required intubation and some time for everything to settle down. (We also gave Icatibant for anyone interested.)
And the thing is, that’s a result exactly consistent with a meta-analysis published in 2018[4]. The authors concluded there was no role for on demand tranexamic acid use in angiooedema. In fact, they even included one small RCT off had to head TXA and Icatibant, which showed a median time to resolution of selling of 2 hours in the Icatibant group, compared to 12 hours for the txa arm.
So, have we found another use for TXA, to get me closer to Pete‘s impossibly optimistic target of ‘101 uses’? Probably not, but it was an interesting case to stimulate me reading up on an area of literature that I otherwise would have left untouched.
I hope you’ve enjoyed me sharing it with you.
References
- Yartsev A. Intepretation of abnormal ROTEM data. DerangedPhysiology.com. Accessed 22 October 2019. Available at URL: https://derangedphysiology.com/main/required-reading/haematology-and-oncology/Chapter%201.2.0.1/intepretation-abnormal-rotem-data
- Raja et al. Acad Emerg Med 2017
- Zirk et al. J Craniomaxillofac Surg 2018
- Wand et al. Chest 2018.
- Wintenberger et al. Clin Exp Immunol. 2014 Oct; 178(1): 112–117.
- Horiuchi et al. J Cutaneous Immunology and Allergy 2018
Written By Dr Luke Lawton
Director Emergency Services
Townsville Hospital




