This is a review of the updated guidelines on Diagnosis and Management of DVT and PE, which were released in March 2020 by the National Institute for Health and Care Excellence(NICE). They now incorporate the use of age adjusted D-dimers and the PERC(Pulmonary Embolism Rule-Out Criteria). They cover the management of different causes of thromboembolism and now describe the use of DOACs for interim and long term anticoagulation. These are very important advances.
We recently had two cases of potential venous thromboembolism, that caused us to question our gestalt decisions, so it is important to have rules that we can use.
CASE 1
A 25 yo woman presents with bilateral ‘burning’-like pain under her rib cage. There is also a pleuritic component to the pain. Her past medical history includes an unprovoked pulmonary embolism, diagnosed on V/Q, for which she had been anti coagulated. The course of anticoagulation had been completed several months previously. She also has symptoms that may be associated with irritable gut syndrome.
Her vitals are: HR of 78 (although it has been and cycles all the way up to 104), Sats are 100% on room air, BP is 128/65 and her respiratory rate is 16. Her examination was normal, with dual heart sounds and a clear chest. Her abdomen was soft and the pain could not be reproduced.
The ECG was also normal.
Our pre-test probably was perhaps emotively, inappropriately raised due to the previous PE. We couldn’t rule her out on PERC score due to her tachycardia. The two level Wells score(see below) was calculated and she scored a 3. We performed a quantitative D-Dimer, which was normal and could rule out PE based on this. Symptoms settled with a PPI and she was discharged.
CASE 2
A 72 year old male presents with a complaint of a swollen left lower leg for the past 3 weeks. It has become increasingly swollen and more painful to ambulate on. His other complaint is a chronic infection of a right hip prothesis, for which he has a long term drain.
The patient, despite the chronic infection on the opposing limb, is very active and has been working on house repairs, for the previous three weeks. There is no history of trauma, however the leg pain appears related to the exertion and time spent working on his house.
His vitals are normal. There is no complaint of dyspnoea or chest pain. His cardiac and respiratory exams are normal. Examination of the painful limb shows that it is a little larger that the other limb at the level of the calf, with some pitting oedema. Pulses are all present and there are no neurological signs.
His ECG is normal.
We do need to consider DVT in this patient. A Well’s 2 point score is calculated and he scores 1 point.
We could do a D-dimer, however given his chronic infection, we decide that it may be inappropriately raised affecting or chances of obtaining an ultrasound in a timely manner. We proceed directly to ultrasound. This is normal and shows some mild oedema. He is given instruction to rest and review with the local doctor.
Guidelines for the Diagnosis and Management of DVT and PE: A summary
SUSPECTED DVT
If we suspect a DVT ie the patient has a swollen and/or painful leg, calculate a 2 level DVT Wells score
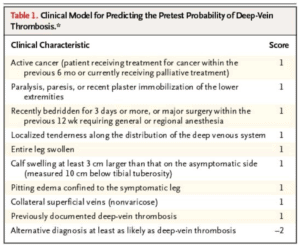
Wells P et al. Evaluation of D-Dimer in the Diagnosis of Suspected Deep-Vein Thrombosis September 25, 2003 NEJM 2003; 349:1227-1235
If the Wells Score is < 1 point, DVT is unlikely
- Perform a Quantitative D-dimer. (age adjust the d-dimer if patient is > 50 years old)
- A normal result means you’re done, stop at that point.
- If it is positive the patient requires an ultrasound. If it cannot be done within 4 hours, provide interim anticoagulation.
If the Wells Score is > 2 points, DVT is likely
- Perform an Ultrasound within 4 hours (if unable to perform within this time offer interim anticoagulation)
- If the ultrasound is shows a DVT, then anticoagulate the patient
- A normal ultrasound requires us to, PERFORM a quantitative D-Dimer
- Age adjust the d-dimer if patient is > 50 years old
- A normal result means we stop
- If positive, the patient requires an ultrasound within 6-8 days(no interim anticoagulation)
- If Ultrasound is not available within 4 hours
- Perform a quantitative D-dimer
- Give interim anticoagulation
- Perform ultrasound within 24 hours
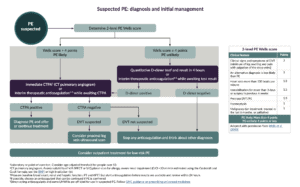
SUSPECTED PE
Calculate a 2 level Wells Score
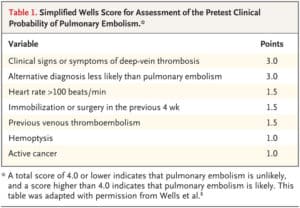
If the Wells Score is < 4 points, PE is unlikely
- Perform a Quantitative D-dimer (age adjust the d-dimer if patient is > 50 years old)
- A normal d-dimer, means we stop
- If positive perform imaging
- CT pulmonary angiogram or V/A SPECT or V/Q planar scan for allergy, severe renal impairment (CrCl <30 ml/min)
- When D-dimer testing is not readily available provide interim anticoagulation
If the Wells Score is > 4 points, PE is likely
- Proceed to imaging (CT pulmonary angiogram or V/A SPECT or V/Q planar scan)
- When a PE is detected anticoagulate
- If negative and a DVT is suspected perform leg ultrasound. If negative stop.
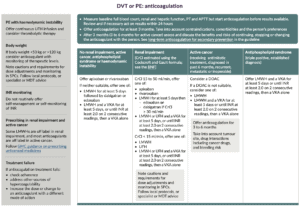
Anticoagulation
When commencing any anticoagulation perform the following blood workup:
- Full blood count,
- Renal and hepatic function
- Prothrombin time (PT)
- Activated partial thromboplastin time (APTT)
Remember that you do not have to wait for the results, before commencing anticoagulation.
Interim Anticoagulation
When choosing interim anticoagulation try to use the same anticoagulant that you might be considering for long term use. DOACs are fine.
Confirmed DVT or PE
Anticoagulation will continue for at least 3 months.
The general recommendation is apixaban or rivaroxaban, with alterations and recommendations based on special groups listed below:
- Patients at extremes of body weight
- Patients with haemodynamic instability
- Renal impairment or established renal failure
- Patients with active cancer
- Triple positive antiphospholipid syndrome.
If neither apixaban or rivaroxaban are suitable consider:
- Low molecular weight heparin (LMWH) for > 5 days followed by dabigatran or edoxaban or
- LMWH with a vitamin K antagonist (VKA) for > 5 days, or until the INR is at least 2.0 in 2 consecutive readings, before commencing a VKA on its own
- Unfractionated heparin (UFH) with a VKA to treat confirmed proximal DVT or PE should NOT be given, unless the person has renal impairment/renal failure
An example of dosages is:
Apixaban: 10mg po bd for 7 days then 5mg bd
Doses need to be modified for Renal and Hepatic impairment as well as the concomitant use of other drug. Please refer to product information.
Rivaroxaban: 15mg PO 12 hourly for 21 days, then 20 mg PO daily. Avoid where creat clearance is <30ml/L. Please refer to product information.
Please refer to infographics produced in the NICE Guidelines for the Diagnosis and Management of DVT and PE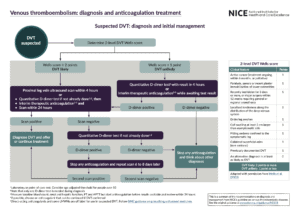
Other blogs that would interest you
V/Q or CTPA in suspected PE in pregnancy
Pulmonary Embolism in patients with Syncope
Thromboembolism in the Post Part period