A 27 yo 34/40 gestation G1P0 patient presented to the Emergency Department with central chest pain, with some radiation to between the scapulae. There was no shortness of breath or diaphoresis, nausea or vomiting or palpitations. The patient did not complain of leg pain. The registrar presented the case to me with the following findings.
Examination
- Vitals: HR 94, BP 120/85-140/90(variable), respiratory rate of 18 and sats of 96% on room air
- Chest was clear
- Heart sounds dual and no extra sounds
- Abdomen was soft
- Calves not tender.
- Bedside U/S showed a live foetus.
Lab tests
- FBC: Hb 119, WCC 8.4 PLT 103
- EUC: Na 139 K 4.5 Cr 44
- Troponin was 4 ng/L (ie., normal)
- D-Dimer 4.67 mg/L (<0.5)
An ECG was performed:
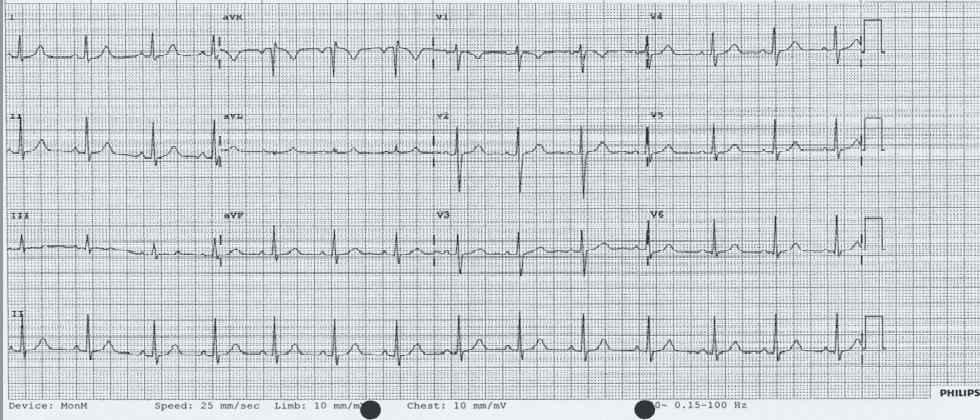
What would you do next?
(a) Serial Troponin
(b) Repeat ECG
(c) Ultrasound of the calves
(d) V/Q or CTPA
(e) Observe
What we did
The pain was very atypical and there was no troponin rise, although a big rise in D-dimer, the patient did not behave like a PE. Our approach was to observe and get a second opinion from the Medical unit.
The patient was observed in short stay and reviewed by the medical unit and discharged home. They did not believe that this was a PE.
What Happened Next?
The patient represented the next day with worsening chest pain that became worst on breathing. However this settled with simple analgesia in the emergency department. The patient also complained of epigastric pain.
Examination
- Vitals: HR 79, BP 130/90, Sats 98% on room air.
- Chest lear HS dual abdo soft, calves non tender
Labs
- FBC: Hb 110, WCC 8.0 PLT 79
- EUC: Na 137 K 3.9 Cr 44
- LFT: Bili 3 ALT 148 AST 141 ALP 108 GGT 23
- D-Dimer 8.38 mg/L (<0.5)
What would you do now?
(a) Admit for Observation
(b) Repeat troponins
(c) CTPA/VQ
(d) CXR
(e) Get urgent O&G Consult
What we did
- A Chest X-ray: There was no abnormality
- Doppler Ultrasound of the legs: No DVT above or below the knee
- Given that all this was normal we performed a CTPA shown
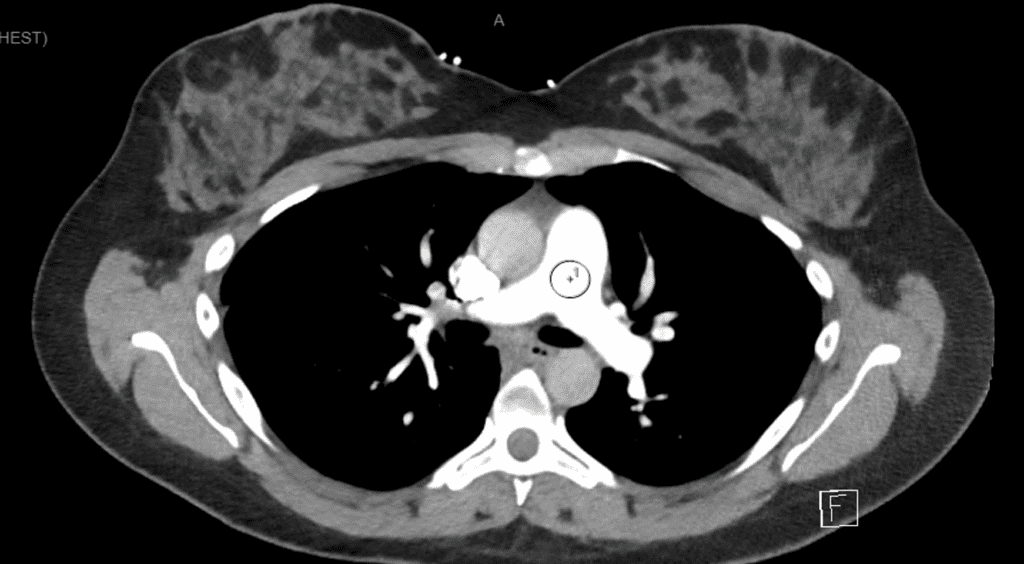
The patient was again reviewed and admitted to short stay unit for observation. Given a further ECG was normal and the CTPA was normal and the patient had no further pain, the patient was discharged.
Obsessive Compulsive Disorder is not always a bad thing……..
I obsessively follow up patients I have seen.
When reviewing this patient a few things stood out for me:
- The blood pressure had been 130/90
- The LFTs were a little deranged
- The patient had a low platelet count.
We recalled the patient.
The patient was well, however we repeated all the labs.
The patients blood pressure was 130/90, sometimes reading 140/90
- FBC: Hb 115, WCC 5.7 PLT 86
- EUC:Normal
- LFT: Bili 3 ALT 127 AST 77 ALP 122 GGT 31
- D-Dimer 7.79 mg/L (<0.5)
Putting it all together the concern was:
- Low platelet count
- Elevated liver enzymes
- Elevated Blood Pressure
Was this HELLP Syndrome?
The patient was admitted under the O&G team and observed for several days. A diagnosis of Gestational thrombocytopaenia was made and the patient discharged after a few days, for a planned delivery the following week.
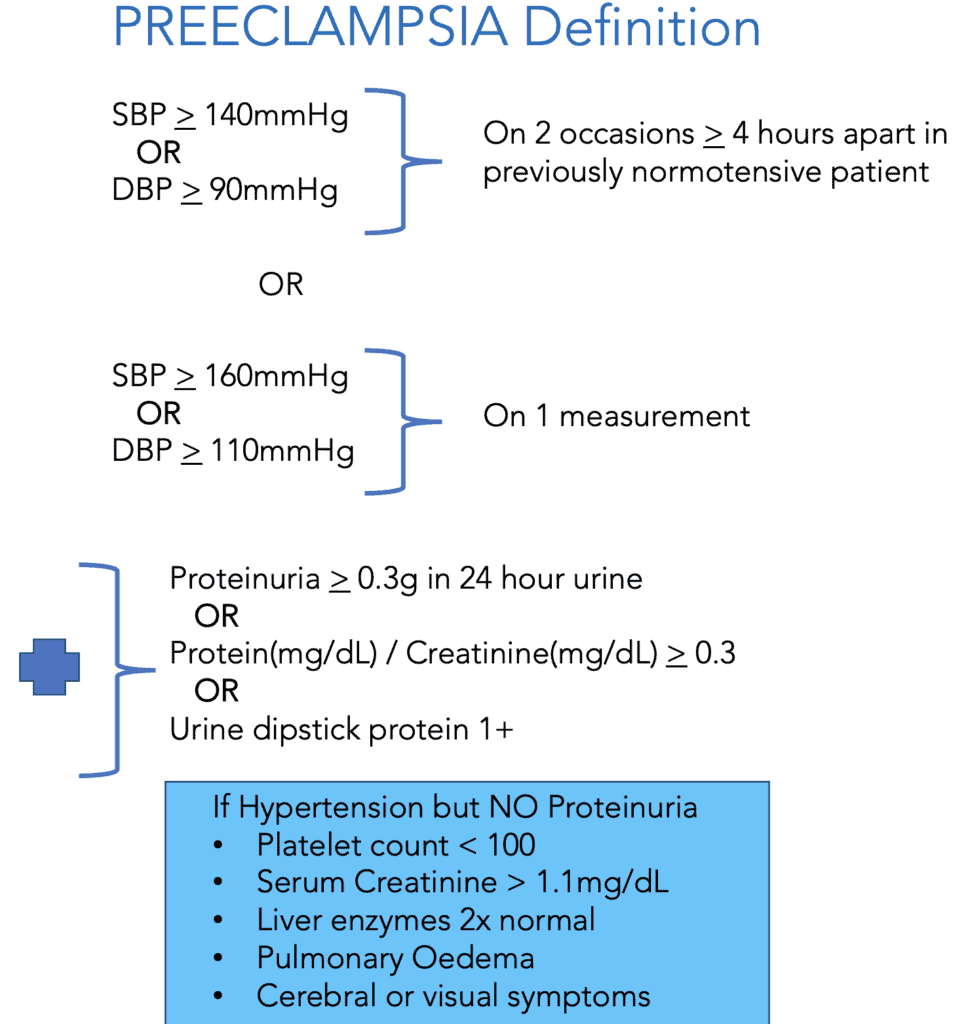
HELLP Syndrome
It stands for HAEMOLYSIS, ELEVATED LIVER ENZYMES, LOW PLATELETS
- Up to 0.6% of all pregnancies,
- Up to 12% of patients with preeclampsia (see below)
- It usually occurs in older maternal age patients
- It tends to occur in > 27 weeks gestation
- Up to 3% maternal mortality and significant morbidity including:
- Placental abruption(16%)
- Acute Renal failure (7%)
- Pulmonary Oedema(6%)
- DIC(20%)
- Associated with 9-24% fetal mortality from:
- placental abruption
- intrauterine asphyxia
- prematurity
Clinical Presentation
The History often includes: Nausea and Vomiting, Epigastric/Abdominal Pain, dyspnoea and oedema
The EXAMINATION may show tachycardia, tachypnoea hypertension and signs of dehydration.
Investigations
- FBC- looking at haemolysis and thrombocytopaenia
- Blood Film- Shistocytes, helmet cells, burr cells
- COAGs
- Fibrinogen Levels- usually decreased
- D-Dimer- Usually increased due to fibrinolysis/DIC
- LFTs
- Increased ALT/AST
- Increased LDH
- Increased Bilirubin
- EUC
Classifications
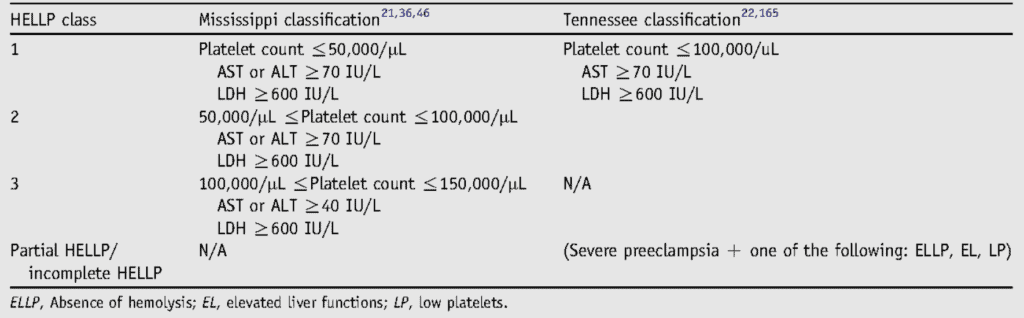
There are two main classifications for HELLP that describe it’s severity.
MISSISSIPPI CLASSIFICATION: It divides HELLP into 3 classes based on platelets, AST, ALT and LDH. Class I is most severe.
TENNESSEE CLASSIFICATION: Describes HELLP as complete or partial. The partial classification includes:
- ELLP: Elevated liver enzymes and thrombocytopenia, but no haemolysis
- EL: Elevated liver enzymes.
- LP: Thrombocytopaenia
- HEL: Haemolysis and liver dysfunction
Management
- IV fluids
- Seizure Prophylaxis
- IV Magnesium Sulphate until 24 hours after delivery
- 6g loading over 20 minutes
- 2g/hr maintenance
- IV Magnesium Sulphate until 24 hours after delivery
- Blood Pressure Control
- Use Labetalol or Hydralazine
- Aim for SBP < 160 and DBP < 105
- Delivery or Steroids
- At > 34 weeks amn unstable=delivery
- At 24-34 weeks and stable= stable then steroids and plan
Potential Complications
Maternal:
- DIC, bleeding and haemolysis
- Pulmonary oedema, PE
- Cardiac ischaemia and arrest
- Seizures
- Renal Failure
Neonatal:
- Thrombocytopaenia
- Intrauterine growth retardation and prematurity.