The Glascow Coma Score(GCS) has long been used as a marker of brain injury severity, following trauma, with a score of 8 or less indicating a more severe injury and scores of 14-15 indicating a milder injury. However there is a real change of delaying investigations and definitive care if this is all we base our prediction on. Perhaps it is a time to challenge old norms and accepted ways of doing things, if it improves patient care.
The GCS when introduced in 1974, was an accepted simple clinical means of recording the level of consciousness with good inter-observer reliability and allowed serial assessment of patients with potential subdural or extradural haemorrhages, that might have required surgical intervention. A few years later it was adopted as a prediction tool. It was never intended for use as a sole predictor. Since those days, we have the capacity to perform CT scans even in some of the smallest centres, which allows visualisation of injuries. We need to beware that we don’t delay the investigations based on a sole measure of GCS.
Fitzgerald et al (1) recently commented on our continued use of GCS, especially when 8 or less, to dichotomise between severe and other traumatic brain injury, in a way in which it was not originally intended. The result can be a delay in investigation and treatment of patients, who may have rapidly evolving injuries.
GCS has served us well as a simple marker, easily and reliably reproducible. However the prediction of mortality and unfavourable events( vegetative state or severe disability) is not always linear. An example of this is the paradoxical finding that patients with a GCS of 4 have a higher mortality than those with a GCS of 3 (2).
Is there a better way of predicting? Are there other markers that we can use separately or in combination with GCS to give us a greater ability to predict? Is there a search for brain injury markers, that can assist us? We have available right now, the pupillary response. This can be of great value in our patient assessments.
What does pupillary response tell us?
In a recent review (3) where data was examined from two major databases on head injury, the CRASH(Corticosteroid Randomisation After Significant Head Injury) (4) and the IMPACT (International mission for program and Clinical Trials in TBQ) (5), pupillary response was found to be a good predictor of mortality.
| No of pupils reactive | Mortality |
| 2 | 16% |
| 1 | 38% |
| 0 | 59% |
As might be expected unfavourable outcomes increased as pupillary reactivity deteriorated. As might be expected pupillary reactivity mirrored GCS. However this was not always a linear relationship, with occasions of non-reactive pupils at higher GCS reflecting higher mortality (Fig 1). These are the cases, where GCS alone, may lead to delay in investigation. Note in the figure below the increased mortality, in patients with a GCS greater than 13-15, but non-reactive pupils.
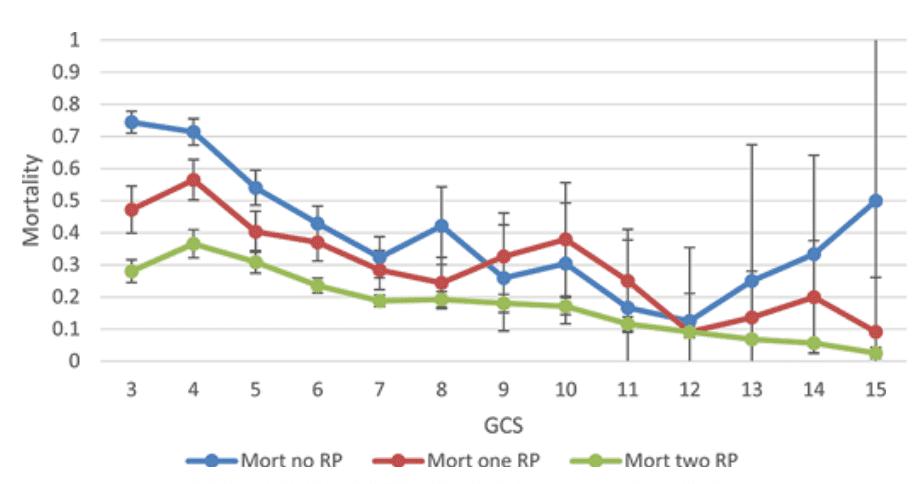
Non-reactive pupils increase the mortality as well as the risk of an unfavourable outcome significantly.
Brennan et al (3) propose the combination of GCS and a Pupillary Reactivity Score(PRS). In this system the GCS and the PRS is added. The PRS is determined by the number of pupils that are reactive ie., 2 pupils unreactive scores a 2, 1 pupil unreactive scores a 1 and 0 pupils unreactive scores a zero.
When the two scores are combined, it appears that there is a smoothing of the curve shown in figure 1 and a more predictable outcome Fig 2.
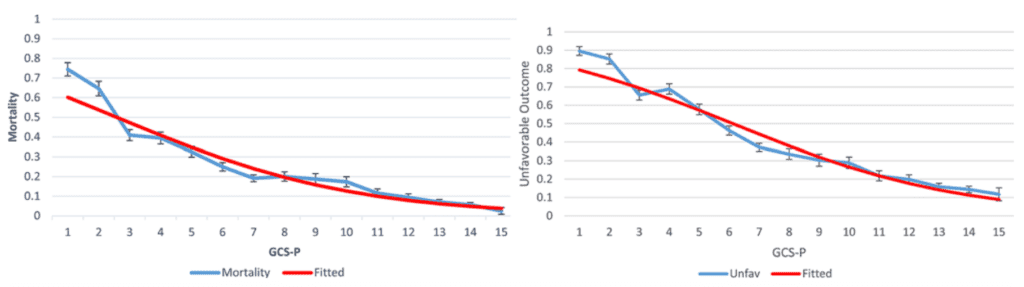
GCS alone may not be an appropriate predictor of severity of head injury and prediction of mortality and in some cases may delay our investigation of patients who are classified as a non-severe injury. Certainly mechanisms of injury will lead quickly to CT imaging, however in some cases, in an alert patient, this may be delayed. Using pupillary reflexes may add to our toolkit, to prompt a more rapid response.
References
- Fitzgerald M et al. An Initial Glascow Coma Scale score of 8 or less does not define severe brain injury. EMA 34, 459-461, 2022.
- Osler T, et al: The differential mortality of Glasgow Coma Score in patients with and without head injury. Injury 47:1879– 1885, 2016.
- Brennan P, M et al. Simplifying the use of prognostic information in traumatic brain injury, Part 1: The GCS-PUpils score: an extended index in clinical severity. J Neurisurg 128;1612-1618. 2018
- Roberts I, et al: Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-con- trolled trial. Lancet 364:1321–1328, 2004.
- Marmarou A et al. IMPACT database of traumatic brain injury: design and description. J Neurotrauma 24:239–250, 2007.