A 28 yo patient presents to the emergency department following a syncopal episode. The patient has had a previous syncopal There were no precipitating factors found and the loss of consciousness was sudden with no premonitory symptoms. He now feels normal. He has no other history and his examination is normal.
His ECG is shown below.
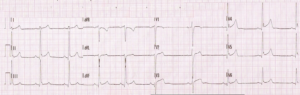
His ECG shows Early repolarisation in the anterior and inferior leads. All laboratory investigations, including a troponin are also normal.
It is decided to monitor the patient given the characteristics of the syncope.
Is Early Repolarisation benign?
Several years ago we began to challenge this belief. Certainly in athletes it may be, however in the general population there has been an association with sudden cardiac death. Now ‘Hot of the Press’ is a new study reviewing the literature. In most cases early depolarisation is benign, however, there are cases where it has been associated with polymorphic ventricular tachycardia and ventricular fibrillation.
Below we look at the patterns that allow us to determine when it might be dangerous.
What is Early Repolarisation?
It is an electrocardiographic pattern (Fig 1) defined as: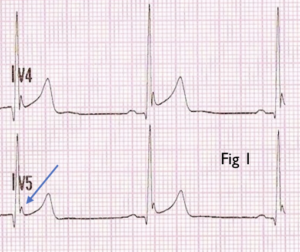
- J-point elevation of at least 1mm in > 1 inferior lead (II, III and aVF) and/or Lateral lead (I, aVL and V4-6) with either:
- QRS slurring (smooth progression of terminal QRS to ST segment) or
- Notching (positive deflection of S wave)
Characteristics of the dangerous pattern
There is an increased risk of arrhythmias and sudden cardiac death when:
- It occurs in young males
- There is a history of syncope. More than 25% of patients with early repolarisation had an episode of syncope
- Inferior early repolarisation patterns are associated with a greater risk of ventricular arrhythmias
- Particular ECG morphologies were associated with increased risk
- ST Segment Morphology: Higher arrhythmic risk occurred in those patients with
- Horizontal/descending ST-Segment in the inferior leads
- When combined with a >2mm J-point elevation, the risk is even higher.
- Notching of the terminal portion of the QRS is associated with a higher arrhythmic risk
- Horizontal/descending ST-Segment in the inferior leads
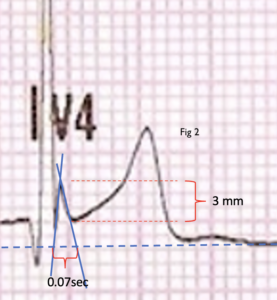
- J-point Amplitude, Duration and Slope (Fig 2)

- J-point elevation of at least 2mm was associated with a higher risk of death
- J-point duration is defined as the distance from J-point onset to where the Jpoint’s tangent intersects the isoelectric line. A longer duration increased the arrhythmic risk. In one study duration was 69.48 vs 35.05 ms.
- The J angle is the angle between an ideal line formed from the jpoint perpendicular to the isoelectric line and the tangent to the J wave. A wider angle (usually > 30 degrees) increases arrhythmic risk.
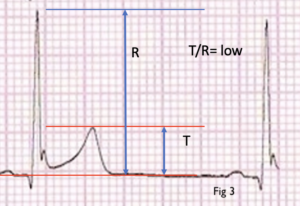
- T wave Morphology
- Usually T waves had low amplitude

- There was a low T wave/R wave ratio in leads II and V5 (Fig 3)
- Usually T waves had low amplitude
- Q waves and T wave inversions were also found to contribute to arrhythmic risk.
- There may be an association with coronary artery disease and other channelopathies.
- ST Segment Morphology: Higher arrhythmic risk occurred in those patients with
Management of Patients with Early Repolarisation
Most patients with isolated early repolarisation require no treatment. Patients who require an implantable defibrillator include:
- Patients surviving ventricular arrhythmias
- Patients with a family history of sudden cardiac death and early repolarisation patterns
- Patients with syncope and early repolarisation
- Those with high risk ECG patterns as discussed above.
Reference
El-Azrak M et al. Sudden Cardiac Death Risk Stratification of the Early Repolarization Syndrome: An Updated Review of the Literature.