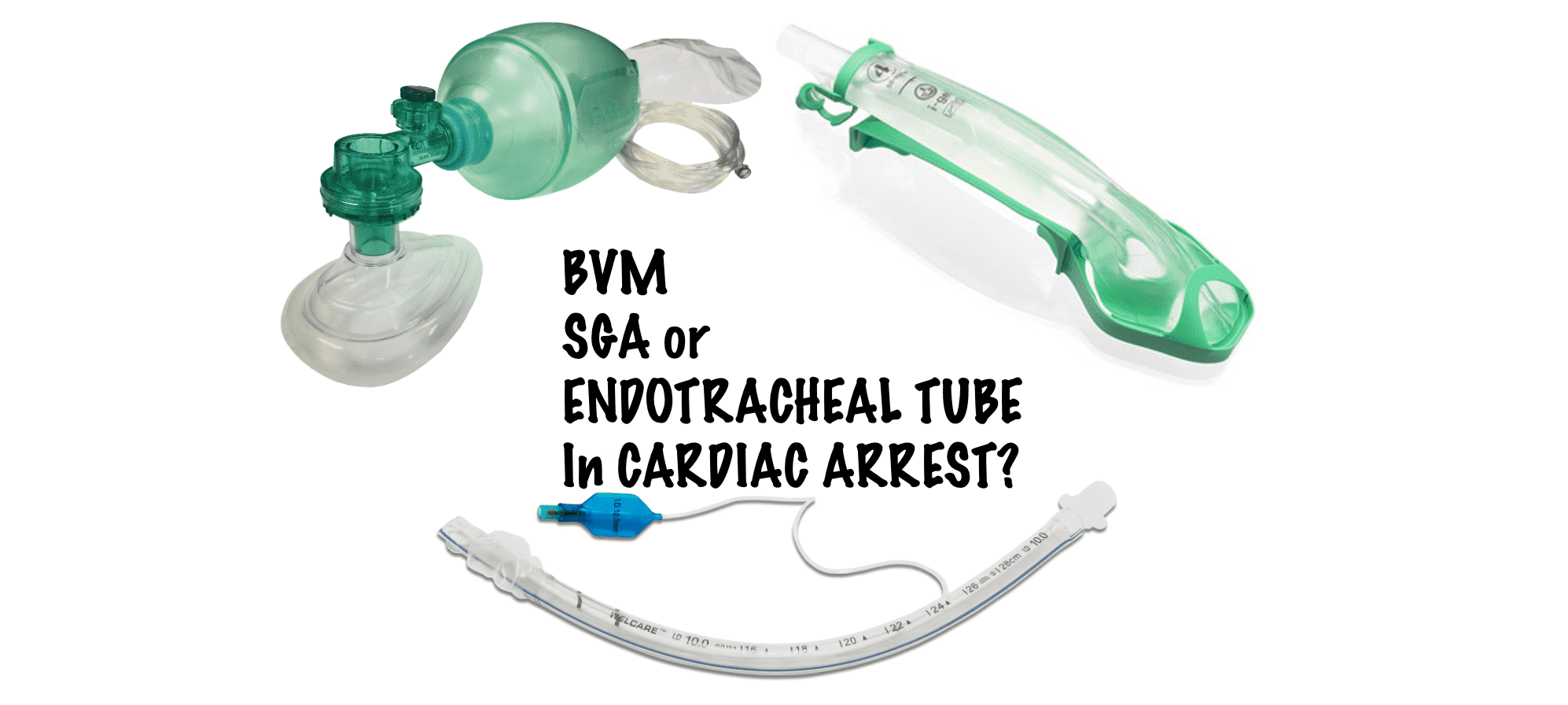
Airway Management during Cardiac Arrest Resuscitation, is still an area that we need to get right. We have seen a move towards bag valve mask(BVM) and supraglottic airways(SGA) in resuscitation, primarily to avoid interruptions to chest compressions. However, new evidence may indicate a reduction in oxygenation with SGA, later in a resuscitation, which may affect outcomes.
Should the airway be managed the same way when we begin cardiopulmonary resuscitation (CPR) as it is later in the arrest?
There is no doubt, that the quality of chest compressions during cardiac arrest and early defibrillation of ventricular tachycardia (VT) or ventricular fibrillation (VF), play a major role in the return of spontaneous circulation (ROSC) and cardiac arrest outcomes. Ventilation and oxygenation of the patient are an important part of CPR. The number and volume of breaths, can determine outcomes, by their effect on thoracic distension and resultant cardiac venous return.
Although the literature shows mixed results, it is generally accepted that no significant difference exits between airway management techniques ie., BVM, SGA, or endotracheal intubation (ETI)(1-3). However some studies using subgroup analysis, do show definite benefits with ETI, including neurologically favourable survival to hospital discharge (4-6).
Should we intubate early or late in resuscitation?
This has mostly been dictated by the need to use the the technique that minimises interruptions to chest compressions. For this reason, the use of ETI has not been as popular early in cardiac arrest. However there is evidence that using video laryngoscopy with a Macintosh blade and bougie allows intubation with minimal interruptions to chest compressions (7).
Should intubation be our preferred ventilation and oxygenation procedure?
Early in resuscitation, four things make a difference:
- Early Defibrillation: Early defibrillation of VT/VF will assist in obtaining early ROSC.
- High quality chest compressions: This means good depth and rate and a good duty cycle, with no unwanted interruptions. It also means that the chest compressions have to be effective and perfuse the coronary arteries. To ensure this occurs we need to monitor arterial blood pressure with an arterial line and alter our compression depth and rate and even position(this may be ultrasound guided) to maximise output.
- Early Adrenaline: Adrenaline is a two edged sword. Survival appears to increase if it is given early ie., the first 10 minutes, however it may be detrimental, if it continues to be given after this initial period.
- Appropriate Ventilation and Oxygenation: Airway in the first 10-20 minutes can be managed with a SGA, or BVM, provided we use end tidal CO2 (ETCO2) to ensure that the patient is being ventilated. However, this may not be the best airway management technique as the resuscitation progresses.
Do the Airway requirements differ after the initial phases of resuscitation?
In a study by Bartos et al (8), they compared the pathophysiological effects of ETI and SGA in patients with refractory cardiac arrest and shockable presenting rhythms, presenting for extracorporeal cardiopulmonary resuscitation (ECPR). The primary outcome was pre-cannulation PaO2 by arterial blood gas. Secondary outcomes included favourable neurological survival at hospital discharge.
What they found was that:
- ETI was associated with a significantly higher PaO2 compared to SGA (71 vs 58)
- ETI had a significantly lower PaCO2
- ETI had a significantly higher pH (7.03 vs 6.93)
- ETI patients were significantly more likely to be eligible for VA-ECMO than SGA patients.
- In patients eligible for VA-ECMO, SGA as the initial airway strategy had an odds ratio of 1.67 for poor neurological outcome compared to ETI (in adjusted analysis)
What can we take from this study?
This study has the significant limitations of non-randomisation and selection bias. What it does look at, is an important area in resuscitation, that we don’t always consider; what happens to the pathophysiology during the time course of resuscitation. Intuitively we know that it must change.
Perhaps we should consider adult cardiac resuscitation as comprising an early and a late phase and that ventilation and oxygenation (as well as Adrenaline) requirements may differ in these two phases:
- Early resuscitation Phase
This is perhaps the first 20-30 minutes of resuscitation(the exact timing of which is unknown), where achieving good cardiac output is the most important determinant of survival. Ventilation and oxygenation can occur with a SGA, if intubation without interrupting chest compressions is not possible.
- Later resuscitation Phase
As resuscitation continues past this first phase, we need to ensure that oxygenation and ventilation are optimised. Barton et al(8) suggest that this is better done with ETI.
An approach I use during Cardiac Arrest with refractory VT/VF?
- Chest Compressions Early. Aim for a good depth (5cm minimum)
- Use a subxiphoid 4 chamber view on ultrasound to ensure compression is occurring in the right place
- Immediate airway can be BVM, with ETCO2(to ensure ventilation), whilst preparing for a SGA (again with ETCO2).
- If video laryngoscopy is available, intubation can be attempted with CPR in progress. If unsuccessful go to SGA
- Shock delivered, with potential repositioning of pads, or in the obese patient using pressure on manual pads at the highest energy level.
- Adrenaline early. Give 3 doses of 1mg of adrenaline and then consider stopping.
- Ultrasound guided femoral arterial line should be established during the rhythm check in the 2nd or 3rd The blood pressure reading can then guide administration of adrenaline or other pressors.
- If resuscitation continues past 20-30 minutes ie., in patients with a refractory shockable rhythm and the patient is not intubated, then proceed to intubation.
More research is still needed.
References
- Jabre P, et al. Effect of Bag-Mask Ventilation vs Endotracheal Intubation During Cardiopulmonary Resuscitation on Neurological Outcome After Out-of-Hospital Cardiorespiratory Arrest: A Randomized Clinical Trial. JAMA 2018;319:779–87.
- Benger JR, et al. Effect of a Strategy of a Supraglottic Airway Device vs Tracheal Intubation During Out-of- Hospital Cardiac Arrest on Functional Outcome: The AIRWAYS-2 Randomized Clinical Trial. JAMA 2018;320:779–91.
- Wang HE, et al. Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72- Hour Survival in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA 2018;320:769–78
- Wang HE, Szydlo D, Stouffer JA, et al. Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation 2012;83:1061–6.
- McMullan J, Gerecht R, Bonomo J, et al. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation 2014;85:617–22.
- Benoit JL, Gerecht RB, Steuerwald MT, McMullan JT. Endotracheal intubation versus supraglottic airway placement in out-of-hospital cardiac arrest: A meta-analysis. Resuscitation 2015;93:20–6.
- Robinson AE et al. First attempt success with continued versus paused chest compressions during cardiac arrest in the emergency department. Resuscitation 2023;186:109726
- Bartos JA et al. Supraglottic airway devices are associated with asphyxia physiology after prolonged CPR in patients with refractory Out-of-Hospital cardiac arrest presenting for extracorporeal cardiopulmonary resuscitation. Resuscitation 2023;186:109769