A 40 yo is brought to the emergency department with the following vitals:
- GCS 4
- SBP 70mmHg
- HR 140
- RR 50
- T 39C
There are no signs of injury. Heart sounds are dual and no extra sounds. There are reduced breath sounds and crepitations in the left base. The abdomen is soft and the patient appears to have peripheral cyanosis. The patient has a known history of IVDU and has been found in a chair, not rousable.
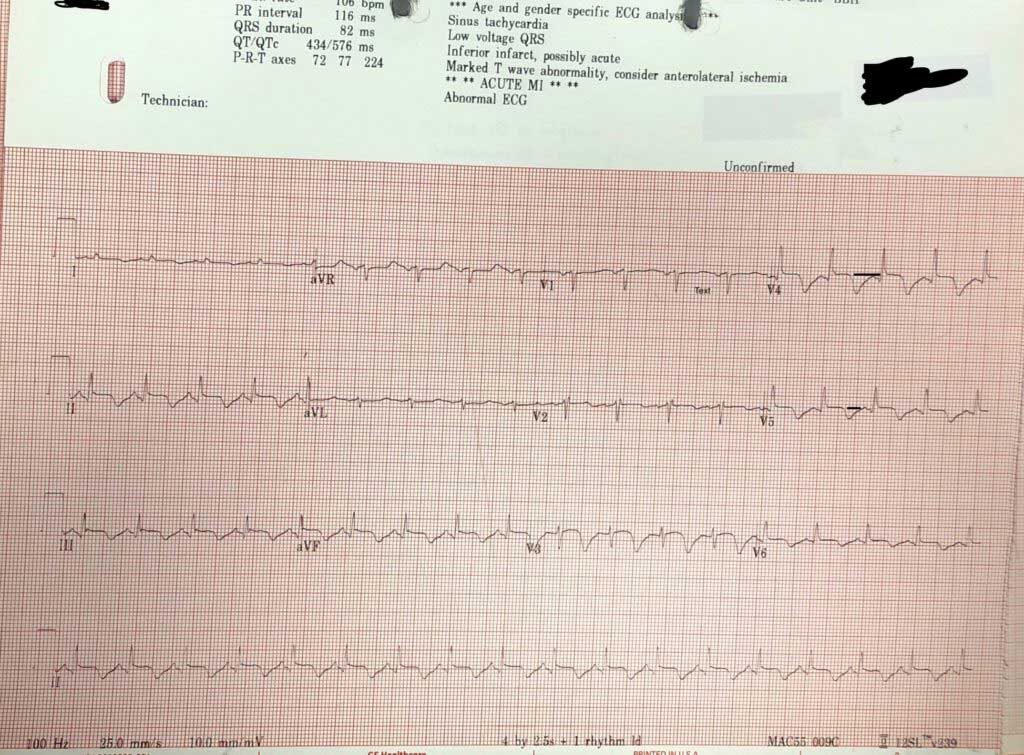
An ECG is done.
- What does the ECG show?
- What are your differential diagnoses for this patient?
- What is the most likely diagnosis?
- The computer says acute AMI. Is it?
If we use the ‘ECG in 20 Seconds Approach’ to describe the ECG, we get the following:
Rate/Rhythm
106
- Is it sinus?– P waves are upright in II and inverted in aVR; Yes
- Is there a P for every QRS? Yes
QRS:
- Is it tall/small?: It’s about right, there is no hypertrophy.
- Is it wide/narrow? It’s narrow
- Is it of abnormal morphology ie., delta wave? No
- Is it clumped?(just incase we miss a Mobitz- but it’s not slow enough) No
ST-T
- Remember the baseline is the T-P line
- If we look we see that there is some ST elevation in some areas of the ECG of about 1mm, although this is difficult to gauge as the T wave goes straight into the p wave.
- The most visible abnormality is the inverted T waves.
What causes inverted T waves?