Adrenaline is the most used drug in cardiac arrest. However we aren’t quite sure what the best dose is. It increases systemic vascular resistance, diastolic blood pressure and cardiac contractility. However it may also worsen brain tissue perfusion. Is one dose of adrenaline better than another? The original work leading to our use of adrenaline was done in 1962, where it was shown to improve survival in cardiac arrest secondary to asphyxia in dogs. The first recommendation for the use of adrenaline in cardiac arrest was in 1974.
Results on outcomes with Adrenaline are conflicting. Some studies show improved survival to hospital discharge and others a negative association with survival.
Jacob et al (1) promised to provide the answer, however the study was underpowered for what we needed.
The Paramedic 2 trial(2); the largest randomised double blind controlled trial to date, with 8014 patients, showed what most other trials have shown, that adrenaline increases ROSC and hospital admission, but it is not associated with an increase in neurologically intact survivors to discharge. In fact, it was associated with a high degree of neurological impairment.
Now, just published, is a systematic review and meta analysis of 18 randomised controlled trials, which combined 21,594 patients. They compared placebo or no treatments, with:
- High dose adrenaline (5mg IV)
- Standard dose adrenaline (1mg IV)
- Adrenaline and vasopressin.
What they found
Return of Spontaneous Circulation (ROSC)
When looking at all the above treatments and comparing them to placebo or no treatment, they found that treatment resulted in increased ROSC.
When comparing high dose to standard dose adrenaline, the high dose adrenaline increased ROSC. The addition of vasopressin made no difference.
Survival to Hospital Admission
High dose adrenaline increased survival to hospital admission, when compared to standard dose adrenaline.
Survival to Hospital Discharge
When compared to placebo or no treatment, there was no improvement to discharge with standard dose adrenaline. The affect of the other treatments was unclear.
Survival and Good Functional Outcome
When compared to placebo and no treatment, standard dose adrenaline had no effect on survival with good neurological outcome. High dose adrenaline had no effect on survival when compared to standard dose.
Shockable vs Non-Shockable Rhythms
There was a definite difference found between these two groups and the use of adrenaline.
In patients with non-shockable rhythms, a standard dose of adrenaline increased ROSC, survival to hospital admission and discharge.
In patients with shockable rhythms a standard dose of adrenaline increased ROSC but had no increase to hospital admission or discharge.
My Take on all of this:
Adrenaline in normal dose improves ROSC.
In Non-shockable rhythms, the early administration of adrenaline improves survival. It should be given early in these patients. In contrast, patients with shockable rhythms should be defibrillated and have CPR, for at least 2 cycles before adrenaline is given.
In all other circumstances adrenaline does not improve survival.
Are we still using too much Adrenaline?
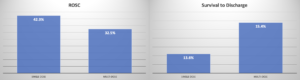
In a recent study(4), they compared single dose adrenaline with the recommended multi dose protocol in 1690 patients.
They found that ROSC was increased in the multi-dose patients [42.3% (380/899) vs. 32.5% (257/791); OR 0.66, 95%CI 0.54–0.81], but there was no significant difference in survival between the two doses [13.6% (122/899) vs. 15.4% (122/791); OR 1.19, 95%CI 0.89–1.59]. Perhaps, a smaller dose is needed.
References
- Jacobs IG. et al. Effect of adrenaline on survival in out-of-hospital cardiac arrest:A randomised double-blind placebo controlled trial. Resuscitation. 82 (2011)1138-1143
- Perkins GD et al. A Randomised Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. NEJM August 13 2018; 379; 711-21
- Epinephrine in Out-of-Hospital Cardiac Arrest. A Network Meta-analysis and Subgroup Analysis of Shockable and NONshockable Rhythms. Chest 2023;164(2):381-393
- Ashburn N P et al. One and Done Epinephrine in Out-of-Hospital Cardiac Arrest? Outcomes in a Multiagency United States Study. Prehospital Emergency Care2023;27:751-757