How do we choose the right pressor in shock? Below is a brief discussion of pressors and their properties as well as 4 cases, where we choose the pressor to use, with reasoning.
If I were to use one general guide, it is, that unless we need to increase the heart rate, then NorAdrenaline, can be used in nearly all cases.
Below are 4 cases to think about. Try them and then scroll down and read on the properties of all these medications.
CASE 1
A 68 yo male is brought to your emergency department in what appears to be septic shock. He has had a recent urine infection. Over the last 24 hours he has become quite febrile and lethargic according to his wife. This morning he felt unwell and felt like he was going to collapse each time he tried to get out of bed.
On arrival he is alert and oriented. He feels unwell. His vitals are as follows:
- Temperature 38.9
- Heart Rate 115 bpm
- Blood Pressure 65/42
- Sats 96% on room air.
The ambulance have given him one litre of Normal Saline and he is on his second Litre.
You make the diagnosis of Septic Shock most likely due to urinary cause and immediately give antibiotics. The second litre of fluids is now in, with no change in blood pressure..
Our Approach:
Given that there is no issue with heart rate at the moment, isoprenaline can be removed. We can also assume no cardiac dysfunction, so we can remove inodilators. This leaves us with:
- Adrenaline
- Noradrenaline
- Vassopressin
The drug of choice to start with is NorAdrenaline. Vasopressin may also be used.
CASE 2
In this case we have exactly the same patient as in case 1 with urosepsis, however, the patient has an added history of atrial fibrillation for which he is on Sotalol. At presentation the patient has a heart rate of 28 beats per minute, and it is a junctional rhythm. He also has acute renal failure and potassium of 7.8mmol/l.
How would you treat this patient’s blood pressure and heart rate now?
This was the case of Septic Shock resulting in acute renal failure, which decreased clearance of Sotalol and resulted in the bradycardia.
Our Approach: A first approach may be to start with isoprenaline and see if there is a rapid change in heart rate and thus blood pressure. If improvement in the heart rate occurs, then Noradrenaline may be added if further blood pressure support is needed. An alternative is to simply commence Adrenaline, which will improve both the heart rate and the blood pressure. Beware in the ischaemic patient.
CASE 3
A 65 yo male is brought in by ambulance. He has had chest pain for the previous 3 hours. He is diaphoretic and looks unwell. His BP is 71/50 and he is speaking in single words, with saturations of 90% on a non-rebreather. His chest examination has widespread crepitations.
He has no relevant past medical history.
Hi ECG is shown below:
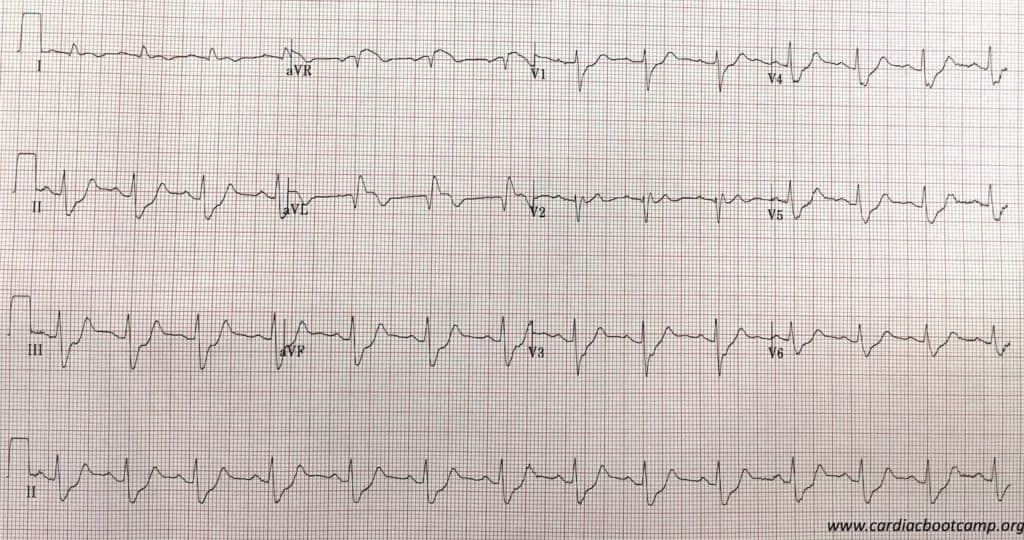
A probable LAD occlusion is diagnosed and that the patient is in cardiogenic shock. Your hospital doesn’t have a Cath lab and so you decide to thrombolyse. However, you also need to sort out the cardiac failure and the blood pressure.
How would you treat this patients’s cardiogenic shock?
Our Approach: GTN is not an option for managing the ischaemia, due to the cariogenic shock. The patient is placed on CPAP to assist with breathing. The optimal blood pressure management for this patient would have been to start NorAdrenaline and then we could add Dobutamine if needed. Milrinone may be a substitute in patients with known poor ejection fraction ie., known significant heart failure.
CASE 4
A 68 yo patient has been sent to the ED from oncology outpatients, where he was receiving chemotherapy. He has a sinus tachycardia of 132, pleuritic chest pain and a tender right calf and his saturations are 92% on room air. On arrival back into the ED following a CTPA, which confirmed a larger central pulmonary embolism, his heart rate stays at 130bpm, his saturations drop to 88% on 6 L of oxygen and his blood pressure is now 68/36.
How would you treat this patient’s blood pressure now?
Our Approach: This is a patient with hypotension secondary to pulmonary embolism and there would be an expected increase in pulmonary vascular resistance. The performance of the right ventricle may be affected. The definitive treatment is thrombolysis, however if the blood pressure is controlled, anticoagulation is also possible (Read more on Pulmonary Embolism)
We started with intravenous fluids in this patient however, to much fluid can be harmful here, especially if there is a suspected right ventricular dysfunction. Volumes should be limited to 250-500 mL. Remember that fluid does very little when ‘the pipes are blocked’ by a clot.
Noradrenaline is the preferred agent in most cases, primarily as it is effective in increasing the BP, and doesn’t result in tachycardias, as might occur with Adrenaline. It is also less arrhythmogenic. It can result in a small increase in pulmonary vascular resistance, however not as much as Adrenaline. Once Noradrenaline is commenced, if the patient still has hypotension, Dobutamine can be added. Beware to start with noradrenaline, as although Dobutamine increases myocardial contractility, it also has an initial vasodilatory effect and can make hypotension worst if given on its own.
An alternative medication is Vasopressin as it has no effect on pulmonary vascular resistance.
Vasopressor vs Inotrope?
A Vasopressor increases systemic vascular resistance and an Inotrope increases cardiac contractility A third property to consider is that some medications result in Vasodilation. Some of these medications also have potentially significant side effects. Perhaps the most important is a risk of arrhythmias. A second but also very important effect to consider, is the effect on the right ventricle via pulmonary vascular resistance.
I will not be discussing Dopamine as part of these as it is both highly arrhymogenic and increases pulmonary vascular resistance. The medications we will be looking at include:
- Adrenaline
- Noradrenaline
- Dobutamine
- Milrinone
- Isoprenaline
- Vasopressin
α1 = vascular(arterial) smooth muscle
β1 = Heart: Increases rate and force of contraction
β2 = Bronchial Smooth muscle dilatation
INOPRESSORS: Adrenaline and NorAdrenaline
Adrenaline (αβββ)
It is a non-selective adrenergic agonist, that is both a chronotrope and inotrope. It acts on α and β receptors. At low doses, it acts on β2 receptors causing vasodilation. At higher doses its effect are on α1 and β1, resulting in positive inotropy and vasoconstriction (of peripheral vasculature and pulmonary arterial and venous circulation). It’s use is mostly in anaphylaxis and cardiac arrest as other drug combinations have been found to be better for both septic and cariogenic shock.
NorAdrenaline (αααβ)
It acts on vascular α1 adrenergic receptors, causing vasoconstriction and thus increasing systolic and diastolic blood pressures. It has chronotropic effect at high doses. It can cause tachycardia and increase myocardial oxygen demand. It is the first line management of septic shock and may be used with other medications.
INODILATORS: Dobutamine and Milrinone
Dobutamine (αββ)
Dobutamine, a synthetic catecholamine, acts on β1 receptors increasing cardiac contractility. It also has α1 and β1 effects on peripheral vasculature resulting in vasodilatation at lower doses, thus increasing cardiac output. At doses above 5mcg/kg/min it can result in vasoconstriction. It is usually used with an inopressor in cardiogenic shock. Higher doses of dobutamine is not preferred in patients with recent myocardial ischemia, as it can increase myocardial oxygen demand and induce tachycardia.
Milrinone
It is a Phosphodiesterase Type 3 inhibitor(PDE3) used as an inotropic agent in patients with cardiogenic shock. It inhibits PDE3, which results in more calcium ions entering the myocardial cell, increasing cardiac contractility. It also acts on peripheral and pulmonary vasculature leading to vasodilatation as well as inotropic effect. It does not act on the beta adrenergic pathway. Another feature of the mechanism of action of milrinone is that the same intracellular processes is activated in smooth muscle cells of the peripheral and pulmonary vasculature, leading to a net vasodilatory effect in addition to its positive inotropic effect.
In a sub-group analysis of the OPTIME-CHF trial, it was found to increase mortality in patients with heart failure of ischaemic origin.
Isoprenaline (ββββ)
It acts on β1 and β2 receptors and increases heart rate and contractility. It’s main use is in significant heart blocks and bradyarrhythmias.
VASOPRESSOR: Vasopressin
Vasopressin (V1 V2)
Vasopressin acts on V1 and V2 receptors leading to vasoconstriction and increasing systemic vascular resistance. It also acts to increase renal water absorption. It may also have an effect on pulmonary vascular dilatation. It is a pure vasopressor and has no inotropic or chronotropic effect.
It has been used in cardiac arrest, but is primarily used in cases where there is shock secondary to vasodilatation, such as in septic shock.
| DRUGS + Receptors | WHEN TO USE | SIDE EFFECTS |
|
ADRENALINE α+++++ |
Cardiac Arrest Anaphylaxis Shock (cardiac/vasodilatory) Bronchospasm Bradycardia |
Arrhythmogenic ++ Pulmonary Vascular resistance -/+ |
|
NORADRENALINE α+++++ |
Shock (cardiac/vasodilatory) |
Arrhythmogenic + Pulmonary Vascular resistance + |
|
DOBUTAMINE α+ |
Low cardiac output: -heart failure -cardiogenic shock -sepsis leading to myocardial dysfunction |
Arrhythmogenic ++ Pulmonary Vascular resistance – |
|
MILRINONE cAMP |
Low cardiac output states in heart failure |
Arrhythmogenic + Pulmonary Vascular resistance – |
|
ISOPRENALINE β1+++++ |
Bradycardias |
Arrhythmogenic + Pulmonary Vascular resistance nil |
|
VASOPRESSIN V1 V2 |
Shock (cardiac and vasodilatory) |
V1 V2 |
References
- De Baker D et al. Comparison of Dopamine and Norepinephrine in the treatment of shock. N Engl J Med 2010; 362:779-789
- Levy B, et al. Comparison of norepinephrine-dobutamine to epinephrine for hemodynamics, lactate metabolism, and organ function variables in cardiogenic shock. A prospective, randomized pilot study. Crit Care Med. 2011;39:450–5.
- Tarvasmaki T, et al. Current real-life use of vasopressors and inotropes in cardiogenic shock – adrenaline use is associated with excess organ injury and mortality. Crit Care. 2016;20:208
- Felker GM et al. Heart failure etiology and response to milrinone in decompensated heart failure: results from the OPTIME-CHF study. J Am Coll Cardiol. 2003;41:997–1003.
- Bistola V et al. Inotropes in Acute Heart Failure: From Guidelines to Practical Use: Therapeutic Options and Clinical Practice. Card Fail Rev. 2019 Nov; 5(3): 133–139
- Maggioni AP et al. EURObservational Research Programme: the Heart Failure Pilot Survey (ESC-HF Pilot) Eur J Heart Fail. 2010;12:1076–84