A 28 yo otherwise well patient has presented to the emergency department with an imminent delivery. The baby is delivered and there is some vaginal bleeding post delivery, however it doesn’t appear significant. The patient is complaining that she is feeling unwell. Her heart rate has increased to 142 bpm. Is this a potential haemorrhage to be concerned about?
Postpartum haemorrhage(PPH) is the leading cause of maternal mortality. It’s overall rate is 5 – 15% but most of these cases are minor. It is considered a primary haemorrhage if it occurs within 24hours of delivery and secondary when it occurs after this and up to six weeks post partum. The management of post abortion haemorrhage is similar to PPH.
The definition of PPH includes:
- Blood loss of 500ml or more during puerperium
- Severe PPH is defined as
- a blood loss of 1000ml or more, or
- signs of haemodynamic compromise regardless of the estimated volume of blood loss. This can be as simple as a tachycardia in the example above.
Risk Factors for PPH
Although bleeding disorders, trauma and abnormal placental position such as placenta praevia increase the risks of PPH significantly, most cases have no identified risks. Prevention of bleeding is mostly dependent on the use of oxytocin’s(50% reduction in bleeding) and the appropriate delivery of the placenta.
An Approach to the Management of PPH
Call for Help
If you are in a large tertiary hospital, your patient, unless unstable will be going to the delivery room for the childbirth and it will not be an emergency department issue. If however you are working in a smaller centre, which may or may not have obstetrics services and the delivery has occurred in the emergency department (whether by your team or the midwives), if there is any suspected PPH, the obstetrician on-call should be contacted. In most cases of severe haemorrhage, the patient will need to go to the operating theatre.
Initial Resuscitation
- Insert two large bore cannulas
- Commence IV fluid – 1-1.5 L Normal Saline (warmed)
- Activate Massive Transfusion Protocol (MTP), or if in a centre where there may be delay in obtaining bloods give O Rh(D) negative blood.
Manage the 4 main causes of bleeding
- TONE(70%) (Uterine Atony) is the most common cause of bleeding (70%)
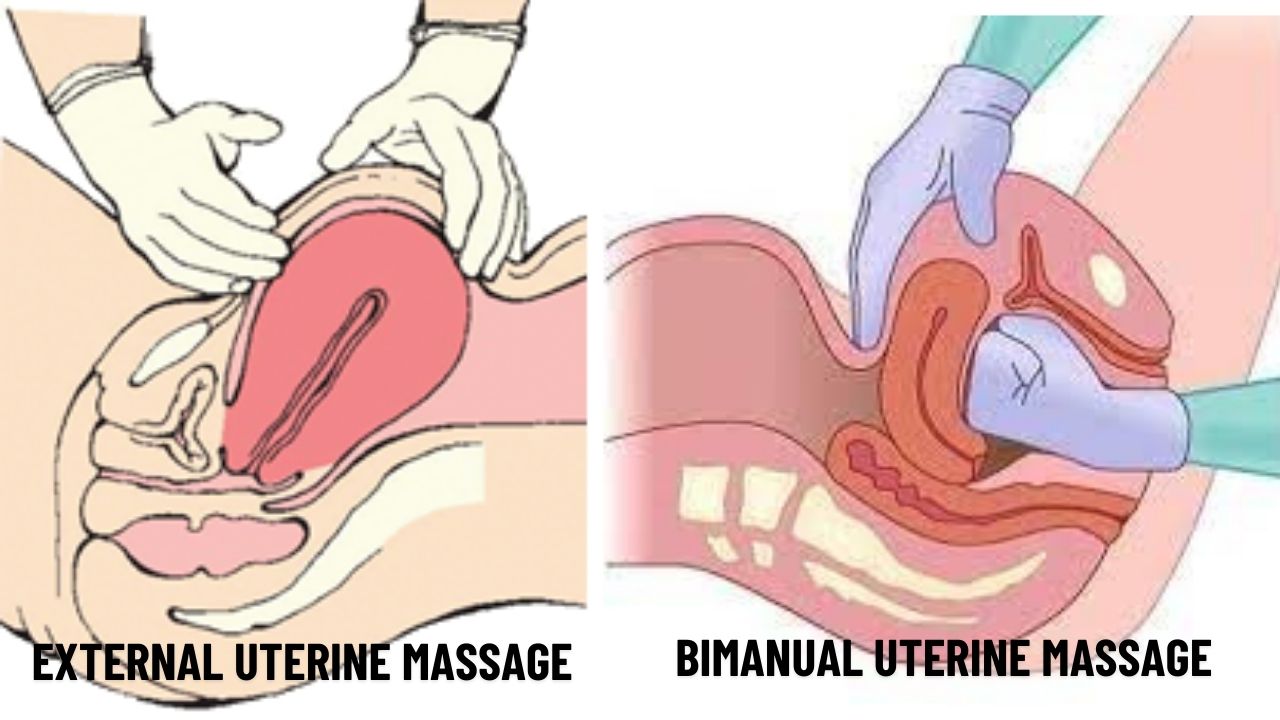
- Massage the uterine fungus externally, however bimanual compression is needed if this doesn’t stop the bleeding
- The Bimanual technique involves external compression with one hand on the abdominal wall and a second hand made into a fist and inserted into the vagina to massage the anterior part of the uterus. Avoid uterine inversion by not massaging downwards.

- The Bimanual technique involves external compression with one hand on the abdominal wall and a second hand made into a fist and inserted into the vagina to massage the anterior part of the uterus. Avoid uterine inversion by not massaging downwards.
- Medications to increase tone: These can be given in a stepwise fashion or in combination.
- Oxytocin (Syntocinon)
- 5IU slow IV. If given rapidly it can result in tachycardia and hypotension. If IV is not available, give 10 U IM.
- Oxytocin in a crystalloid solution infusion. Put 40 U in 1 L normal saline and run in until the uterus is firm, then infuse at 200mL/hr.
- Syntometrine is a combination of oxytocin (5U) and ergometrine 500mcg. It is given IM. Avoid if there is hypertension as it can precipitate eclampsia.
- Misoprostol- 800-1000 mcg rectally. It is equivalent to another dose of Oxytocin. It’s main use is in 3rd stage labour.
- Carboprost (PGF2alpha). Another uterotonic. These drugs can cause severe hypertension and bronchospasm. It can be given in one of two ways:
- 0.25mg IM and repeated up to 2mg , with doses at least 15 minutes apart.
- 0.5mg intramyometrial injection (off label)
- Oxytocin (Syntocinon)
- Massage the uterine fungus externally, however bimanual compression is needed if this doesn’t stop the bleeding
- TRAUMA (20%): Examine the genital tract for lacerations or areas of bleeding. Apply direct pressure or suture. If nothing can be seen, the blood may be in the uterus or the uterus may be ruptured. A rapid POCUS uterine examination may assist.
- TISSUE (10%): Look for retained products. Inspect the placenta to ensure it is complete.
- THROMBIN (1%): This refers to any problems in coagulation
- Tranexamic Acid (TXA) : As per the WOMAN Trial there was a reduction in mortality due to haemorrhage if 1g TXA is given IV over 10 minutes. A second dose can be given in 30 minutes if bleeding has not ceased
- Treat Coagulopathy
- If MTP used give FFP
- Cryoprecipitate for DIC
- Aim for fibrinogen of < 1.5-2g
- DDAVP for VWD
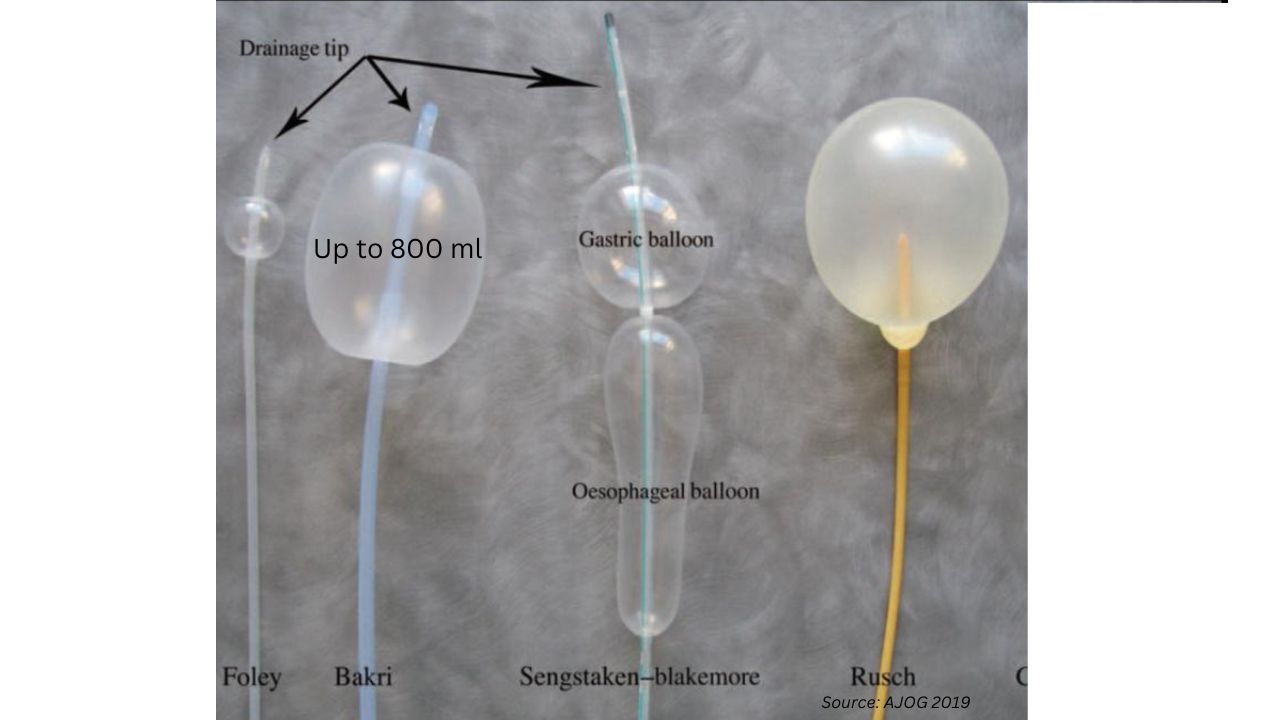
- TAMPONADE and THEATRE: Most patients if continuing to bleed, will need to go to the operating room for surgical procedures such as haemostat suturing, ligation of the uterine arteries, embolisation or hysterectomy. Temporising measures such as tamponade may be used, to obtain some control as the patient prepares for theatre. These include:
- Specific devises such as a Bakri or Rusch balloons
- If specific devises are not available, there is a potential to use a Sengstaken-Blackmore tube and fold the gastric balloon back and inflate the oesophageal balloon.
- Using a single Foley catheter, is of no use as its maximum volume is 80ml as compared to a Bakri balloon whose volume is as much as 800ml.

Blood loss from PPH is an emergency. The placental bed is very vascular and at birth blood flow approaches 750ml/min. A significant bleed for three to four minutes can represent 30-40% blood loss. Our approach must be rapid and coordinated.
- Start tow ABC, give some fluid and call for blood/ activate MTP as needed.
- Start Uterine massage to increase tone (external and then move to bimanual)
- At the same time, if the placenta has been delivered, have someone check to see that it is intact.
- Ensure all the oxytocics are given: Oxytocin or Syntometrine, Misoprostol and Carboprost
- Give TXA
- Look to ensure there is no trauma or tear that needs repair
- Remove any products of conception
- Ensure blood and coagulopathy is treated
- Tamponade the bleed.
References
- Management of Post Partum Haemorrhage: Clinical Guidance Statement 2021 RANZCOG (C-Obs 43)
- Georgiou C. Balloon tamponade in the management of postpartum haemorrhage: a review. BJOG 2009; 116(6): 748-57.
15 min reading time