Cervical spine injuries in children are uncommon and radiation risk from CT scans can be significant. We don’t have specific paediatric prediction rules for potential cervical spine injuries in children.
We review the new cervical spine injury prediction rule for children.
The Paper:
Leonard J C et al. PECARN prediction rule for cervical spine imaging of children presenting to the emergency department with blunt trauma: a multicentre prospective observational study. Lancet Child Adolesc Health 2024; 8: 482–90. doi:10.1016/S2352-4642(24)00104-4
Listen to the EM Mastery PODCAST on this topic Interview with PEM Physician Dr Clair Wilkin Marshall
What They Did
In this study they derived and validated a clinical prediction rule for cervical injury in children.
- This was a prospective observational study, of children 0–17 years with known or suspected blunt trauma presenting to one of 18 PECARN affiliated level-1 paediatric trauma centres.
- 9 sites were used for the derivation cohort and 9 sites for the validation cohort.
- 22 430 children with known or suspected blunt trauma were enrolled
- 11 857 in the derivation cohort
- 10 573 in the validation cohort.
- 433 (1·9%) of patients had a confirmed cervical spine injury.
Inclusion Criteria:
- Evaluation by a trauma team;
- Cervical spine imaging performed at the participating hospital
- Cervical spine imaging performed before transfer to the participating hospital.
Exclusion Criteria:
- Penetrating trauma (eg, gunshot or stab wound).
The treating clinician completed an electronic questionnaire to complete. The questionnaire provided examples of substantial injuries for each
body region. It allowed the gathering of information about predetermined potential cervical spine injury risk factors including:
- predisposing conditions,
- injury mechanism,
- neck and neurological complaints, and
- regionalised physical examination findings (head, torso, and spine).
Primary Outcome
Cervical spine injury within 28 days of trauma requiring inpatient admission or surgical intervention.
Cervical spine injury was defined as including:
- fractures or
- ligamentous c-spine injury,
- cervical intraspinal haemorrhage or
- vertebral artery injury, or
- cervical spinal cord injury,
Patient Follow up
Research personnel who categorised the outcome were blinded to the clinical predictors for that patient.
A cervical spine injury was determined to be present or absent by:
- Reviewing the hospital medical record, 21–28 days following the emergency department visit
- Reviewing C spine imaging reports and surgical consultation notes
- A paediatric neurosurgeon, reviewed neck imaging reports and surgical consultation notes to confirm cervical spine injury.
- If there was inconsistent documentation, the treating spine surgeon was contacted for final determination of injury status.
- In patients where no imaging had been performed, guardians were contacted by telephone to determine whether a cervical spine injury was subsequently diagnosed.
The prediction rule was determined from data from the derivation cohort.
What They Found
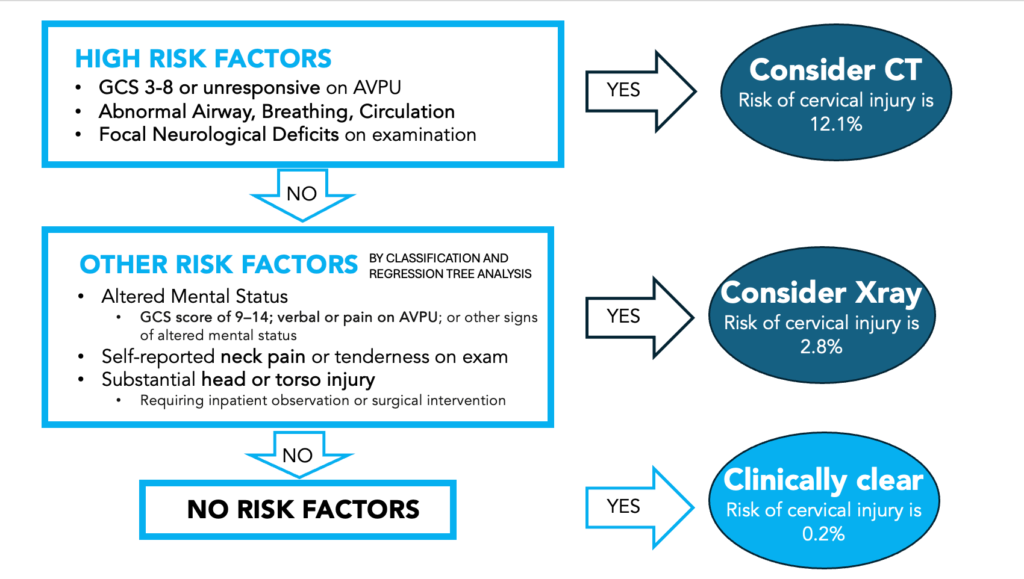
High-risk clinical examination factors were found in 928 children and included:
- Glasgow Coma Scale (GCS) 3–8 or
- unresponsive on the Alert, Verbal, Pain, Unresponsive scale (AVPU) of consciousness;
- Abnormal airway, breathing, or circulation;
- Focal neurological deficits including paresthesia, numbness, or weakness.
The remaining 10 929 children were analysed for variables associated with non-negligible risk of cervical spine injury, identifying an additional five classified those at risk for cervical spine injury They were:
- neck pain,
- altered mental status (GCS score of 9–14; verbal or pain on AVPU; or other signs of altered mental status),
- substantial torso injury,
- substantial head injury, and
- posterior midline neck tenderness
These were combined into a nine-factor prediction rule, which had a
- sensitivity of 94·3% (95% CI 90·7–97·9),
- specificity of 60·4% (59·4–61·3), and
- NPV of 99·9% (99·8–100·0).
29 children with none of these risk factors were found to have cervical spine injuries. On review 20 had at least one risk factor. None of the remaining nine children with cervical spine injuries that were missed.
Mechanism was not used to assess the risk.
My Take on This
This is a well done study, by the clever PECARN group of researchers. It provides a simple tiered approach to determining who needs imaging and what kind of imaging is needed. It has a high sensitivity and a very high NPV. The findings still need to be validated outside the USA.
The aim of this study was to reduce the amount of imaging, especially of CTs, as they pose a significant radiation risk and an increased incidence of cancer. There is no doubt that the high risk group, in this study, would most likely receive CT imaging. However, in the lesser risk group, that imaging may now be replaced by plain C-spine series x-rays….. which concerns me a little.
Here’s how I see this playing out (listen to the Podcast on this topic this month, where I interview PEM Dr Claire Wilkin-Marshall):
- If I have a child that is in a coma, or needs me to intervene with airway, or breathing or circulation, I’m sure that I’ll be doing a CT Crain and even a cervical spine on these patients.
- I think it will be difficult to ascertain a focal neurological deficit in younger children
- A substantial head injury, which is one of the lesser risk factors, may end up getting a CT
- If we are now doing more C spine x-rays, which creates some issues in my mind:
- Will this increase imaging in the lesser risk group, with plain films.
- Reading plain x-rays of the under-developed C spine may pose a problem. I haven’t looked at an adult or paediatric C-spine x-ray in quite a few years. I’m sure that neither has the radiologist. Could this result in overcalling of the films with repeat films necessary, or even progression to CT, or or MRI, even worse, incorrectly clearing the spine?
- What I usually see at the bottom of the x-ray report is some comment on correlating it with the clinical picture and that CT or MRI may be needed.
- This has the associated problems or availability of MRI and the need for sedation.
- Will this in fact increase the amount of imaging I’ll be doing?
- How useful is the plan C spine x-ray, especially in the very young child? Probably not that useful.
- There is no mechanism incorporated into this rule and this was done on purpose. However the mechanism, for me becomes very important as some injuries are of such high risk, that we may be doing a CT early and others of such low risk, that I won’t image.
I await the validation study.
(15 min read)