You review her in the triage room as the department is filled to capacity. The vitals are all normal but the child looks tired and has some coryza symptoms. You ask the resident to get the rest of the story and show you an ECG.
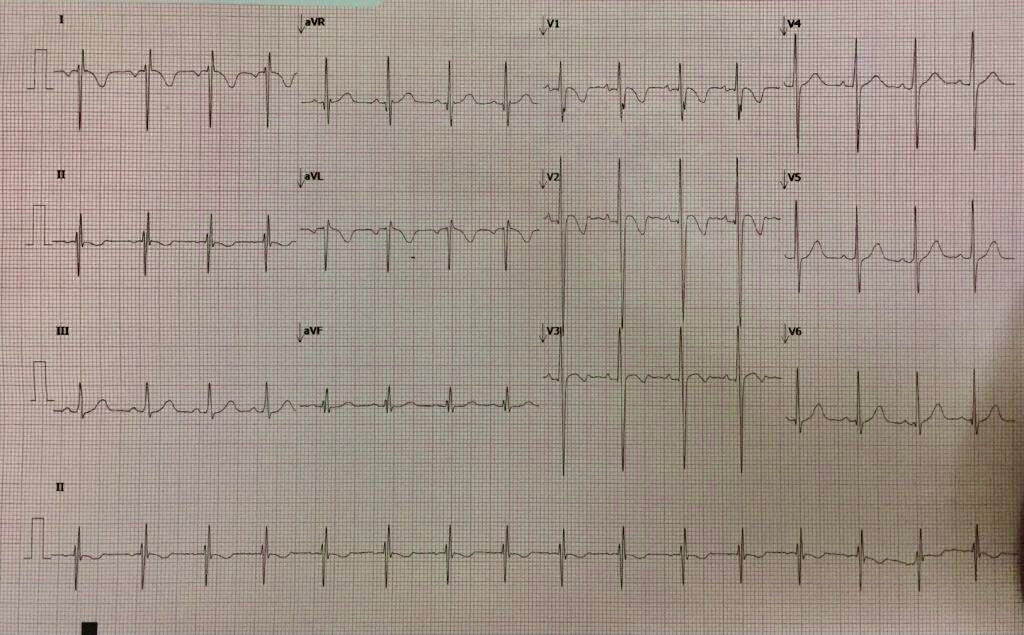
The resident brings you the ECG shown below. What is your comment on this ECG?
ECG Interpretation
At first glance: There is T wave inversion in anterior leads but you would expect this in a young girl. There are however T waves inverted in the lateral leads…….STOP. Let’s go over the ECG in a systematic fashion.
Is it sinus rhythm? For it to be sinus, the p wave in II must be upright and the p wave in aVR inverted. This is not the case. Now look at lead I, The p waves are inverted and they should be upright.
Two things give you this pattern:
- Limb lead reversal and
- Dextrocardia
This ECG is the result of limb lead reversal.
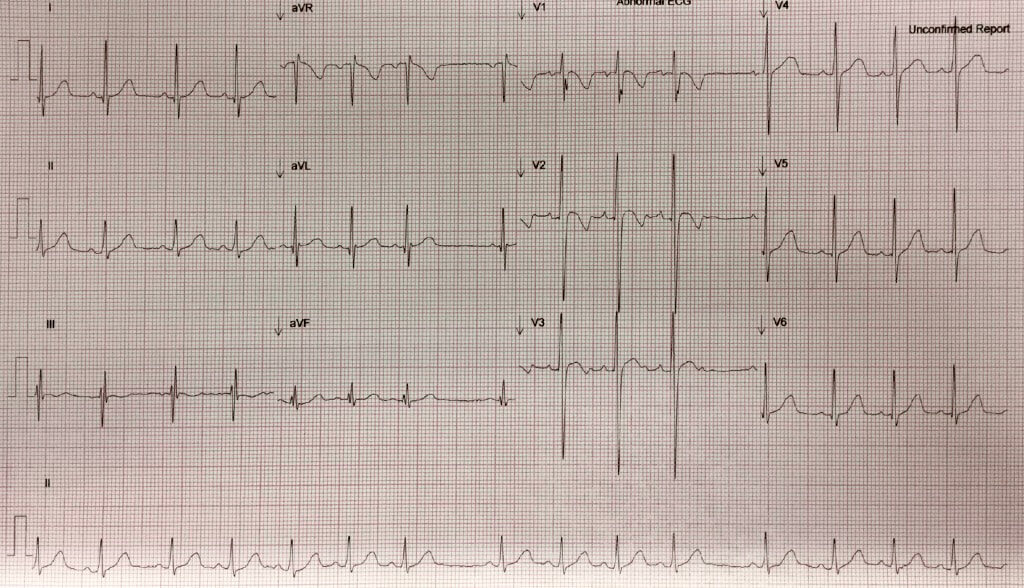
You have the ECG redone. The ECG is shown below. How would you comment on this?
ECG Interpretation
Hr : 90 bpm
Is it sinus? YES- p waves inverted in aVR and upright in II.
There is a sinus arrhythmia, but always a p wave for every QRS
The QRS complexes show a RIGHT to LEFT Heart predominance transition, which is expected.
There are no ischaemic or other ST changes and the T wave inversions in the anterior leads are normal for this age group, although you would expect them to be flipping back upward at about this age. There are some U waves to be seen in the anterior leads, which may suggest hypokalaemia.
The Intervals show a normal PR interval, however the QT interval looks prolonged and when the QTc is measured, it is 480ms.
There is variability in what we consider a normal QTc, however in children above 6 months old an upper limit of QTc is 460ms.
Prolonged QT can lead to Torsades de Pointes, also known as Polymorphic Ventricular Tachycardia. This is usually a self terminating arrhythmia, but can recur. The result may be a loss of consciousness, or even seizure-like activity due to haemodynamic compromise. It can occur repeatedly, or for a single episode.
Why do we correct the QT?
Corrected QT gives us the QT interval at a heart rate of 60 beats per minute. This allows comparison over time at various heart rates.
There are several formulae for calculating the corrected QT. The RR interval is 60/heart rate (seconds)
- Bazett’s formula: QTC = QT / √ RR
- The most commonly used and probably best for heart rates of 60-100
- Fridericia’s formula: QTC = QT / RR 1/3
- This along with the Framingham formula below are more accurate when the heart rate is outside the 60-100 range/
- Framingham formula: QTC = QT + 0.154 (1 – RR)
What are the potential causes of a long QT?
- Congenital
- Congenital Long QT Syndrome
- Myocarditis
- This can have an insidious onset and can be viral or bacterial. It is usually associated with a recent viral illness and it can result in very sick children. The presentation originally may be with ECG changes, but this can progress to heart failure and long term sequelae of dilated cardiomyopathy.
- Electrolyte abnormalities
- Hypo – kalaemia/ calcaemia/ magnesiaemia
- Raised intracranial pressure
- Medications
- Antibiotics mostly macrolides such as erythromycin and clarythromycin
- Antihistamines such as Loratadine
- ADHD medications can prolong QT.
Outcome
We discussed the case with the local paediatrics service for admission and monitoring. The Tertiary Paediatric Cardiology service was involved in this case and they were happy for the child to be monitored in the emergency department for some time and then discharged, for outpatient holder monitor and ECHO.