CASE
A 25 yo male presents to the emergency department with palpitations and shortness of breath.
His vitals are:
- HR 173 bpm
- BP 132/67
- RR 32
- SaO2 82% on room air and 92% of a rebreather mask.
His past medical history is that of depression and obesity. At best estimate he weights approximately 250kg.
On examination he is tachycardic with bilateral full filed lung crepitations ie cardiac failure.
The ECG shows rapid atrial fibrillation.
We will meet this patient again at EMCORE from the point of view of the crashing obese patient and also in Cardiac Bootcamp, in terms of Type II myocardial injury.
Our patient above was 168cm tall and weighed about 250kg giving him a BMI of 88.6 kg/m2
Airway Pearls
The areas we will look at are:
- Difficult Intubation resulting from anatomy and physiology
- Normal airway techniques may not be effective.
- Positioning of the patient is critical- aim for head up.
- Pre-oxygenation techniques are crucial
- Appropriate medication dosing is important
- Video laryngoscopy may provide an edge
- Mechanical Ventilation needs to be tailored
Anatomy and Physiology in the obese patient.
The anatomy and the physiology make every case of intubation a potentially difficult airway and we need to assume that every case will be difficult.
- A BMI greater than 30 kg/m2 is considered obese. BMI’s greater than 40 kg/m2 considered severely CLASS III obese.
- For example a 168cm person weighing 85kg is considered obese. We need to keep some perspective on these. It’s not just the absolute weight. I know a lot of rugby players that fall into that range.
- Obese patients have a decreased overall, lung capacity and an increase in metabolic activity. This results on increased oxygen consumption and an increased work of breathing.
- The adipose tissue produces increased metabolic activity as well as increasing airway resistance and potentially causes increased risk of pharyngeal wall collapse with paralysis.
- The ability to adequately pre-oxygenate give safe apnoea times is affected as the functional residual capacity is also decreased. Safe apnoea times are decreased to one to two minutes.
- The displacement of the diaphragm makes ventilation in the supine position more difficult and can lead to desaturation more readily, in this position.
- Obese patients are more difficult to ventilate and they desaturate far more rapidly.
Airway Techniques and Modifications
- The airway in the obese patient must always be assumed to be a difficult airway. The risk of rapid desaturation is high and the increase in airway resistance makes BVM ventilation more difficult (1,2); a 2 hand technique (2 operator) being required.
- Use a PEEP valve at 10cm H20.
- The use of airway adjuncts, such as nasopharyngeal and oropharyngeal (unless contraindicated) may help with ventilation (3)
- Laryngoscopy can prove difficult due extra adipose tissue resulting in an alteration of the anatomy.
- A predictor of difficult intubation is a large neck circumference and a high Mallampati Score (4).
- Laryngeal masks can be used in the obese patient (5)
- Performing a surgical airway on these patients is extremely difficult due to the inability to identify important anatomical landmarks (6). Bedside ultrasound may assist in identifying the anatomy (7,8)
Correct Patient Positioning is Critical
- Patients should be placed in the upright position, to allow the diaphragm to fall and allow greater ventilation of the lungs.
- If it’s not possible to sit the patient upright eg., in trauma, with cervical precautions, a reverse Trendelenburg position is recommended.
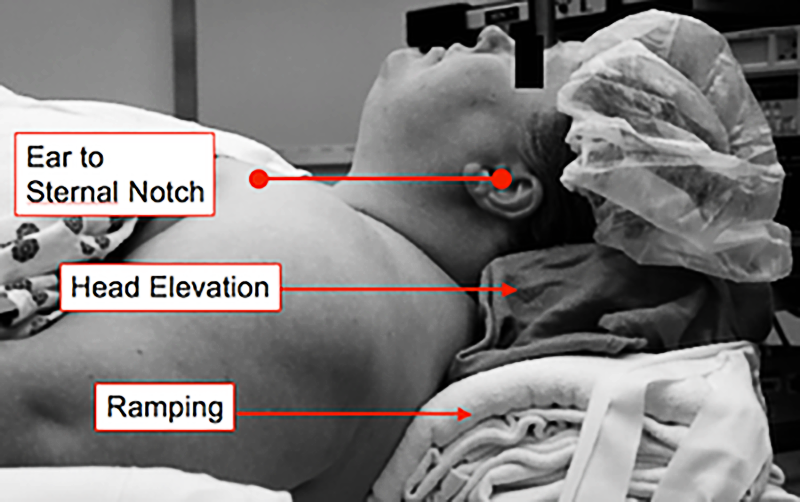
- In preparation for intubation, the ramped, head-up position where the auditory canal is aligned with the sternal notch, provides a better position for visualisation of the glottis. (9,10), with improvements of over 50% when head elevation is used, as compared to supine positioning (11).

Pre-Oxygenation is Crucial
- Given that obese patients desaturate very rapidly, adequate pre-oxygenation is imperative, if time allows.
- Non-Invasive ventilation such as CPAP can improve oxygenation (12,13). A minimum of 5-10 minutes may be needed.
- Apnoeic Oxygenation via high flow nasal prongs should also be used during the procedure.
Medication Dosing in the Obese Patient
The pharmacokinetics of some medications is altered by obesity. Obese patients have a higher glomerular filtration rate, causing renally excreted drugs to have shorter half-lives.
We need to which medications should be given according to ideal body weight versus total body weight doses. Induction and paralysis medications are shown below:
- Propofol: Ideal Body Weight. There is a significant risk of hypotension if larger doses are used.
- Ketamine: Ideal body weight
- Suxamethonium: Total body weight.
- Rocuronium: Ideal body weight. It appears that the duration of action is prolonged if total body weight is used, however the time to relaxation may not be different (14)
Video Laryngoscopy vs Direct Laryngoscopy
- Awake intubation may be an option to consider for the obese patient, assuming they can maintain saturations.
- Normal laryngoscopy may need some modifications including a short handle laryngoscope and larger blade sizes.
- Video laryngoscopes have resulted in better views of the glottis and produced views of the glottis (15,16,17)
Mechanical Ventilation
- Use ideal body weight for tidal volumes of 6-8mL/kg.
- Higher respiratory rates will be needed as obese patients have spontaneous respiratory rates of 15-20 breaths per minute.
- Positioning in the reverse Trendelenburg position may improve oxygenation and ventilation
- PEEP of 10-15cmH20 may be needed.
Summary
- Consider every case a difficult Intubation due to effects on anatomy and physiology
- Increased airway resistance
- Increased tissue results in higher metabolic rates and rapid desaturation
- Increased tissue may cause pharyngeal wall to collapse
- Normal airway techniques may not be effective.
- Two handed BVM should be used
- Airway adjuncts such as oropharyngeal and nasopharyngeal airway may help
- Positioning of the patient is critical- aim for head up.
- Sitting position or head up is better for pre-oxygenation
- Reverse Trendelenburg may assist
- Ramp up and ear to sternal notch positioning for intubation
- Pre-oxygenation is crucial
- Rapid desaturation
- Pre-oxygenate in upright position
- Use CPAP
- Use high flow apnoeic oxygenation
- Medication dosing is important for optimal conditions
- Use total body weight for suxamethonium dosing
- Use ideal body weight for Propofol, Ketamine and Rocuronium dosing
- Video laryngoscopy may provide an edge
- Video Laryngoscopy gives a better view than Direct Laryngoscopy
- Mechanical Ventilation needs to be tailored
- Use ideal body weight for Tidal Volume
- Increase respiration rates are needed.
- Use PEEP 15-20cm H20
References
- Levi D, et al. Critical care of the obese and bariatric surgical patient. Crit Care Clin 2003; 19:11.
- Varon J, Marik P. Management of the obese critically ill patient. Crit Care Clin 2001; 17:187.
- Gerstein NS, et al. Efficacy of facemask ventilation techniques in novice providers. J Clin Anesth 2013; 25:193.
- Brodsky JB, et al. Morbid obesity and tracheal intubation. Anesth Analg 2002; 94:732.
- Zoremba M, et al. Comparison between intubation and the laryngeal mask airway in moderately obese adults. Acta Anaesthesiol Scand 2009; 53:436.
- Aslani A, et al. Accuracy of identification of the cricothyroid membrane in female subjects using palpation: an observational study. Anesth Analg 2012; 114:987.
- Dinsmore J, et al. The use of ultrasound to guide time-critical cannula tracheotomy when anterior neck airway anatomy is unidentifiable. Eur J Anaesthesiol 2011; 28:506.
- Siddiqui N, et al. Ultrasound Improves Cricothyrotomy Success in Cadavers with Poorly Defined Neck Anatomy: A Randomized Control Trial. Anesthesiology 2015; 123:1033.
- Rao SL, et al. Laryngoscopy and tracheal intubation in the head-elevated position in obese patients: a randomized, controlled, equivalence trial. Anesth Analg 2008; 107:1912.
- Collins JS, et al. Laryngoscopy and morbid obesity: a comparison of the “sniff” and “ramped” positions. Obes Surg 2004; 14:1171.
- Lee BJ, et al. Laryngeal exposure during laryngoscopy is better in the 25 degrees back-up position than in the supine position. Br J Anaesth 2007; 99:581.
- Delay JM, et al. The effectiveness of noninvasive positive pressure ventilation to enhance preoxygenation in morbidly obese patients: a randomized controlled study. Anesth Analg 2008; 107:1707.
- El-Khatib MF, et al. Noninvasive bilevel positive airway pressure for preoxygenation of the critically ill morbidly obese patient. Can J Anaesth 2007; 54:744.
- Leykin Y, et al. The pharmacodynamic effects of rocuronium when dosed according to real body weight or ideal body weight in morbidly obese patients. Anesth Analg 2004; 99:1086
- Marrel J, et al. Videolaryngoscopy improves intubation condition in morbidly obese patients. Eur J Anaesthesiol 2007; 24:1045.
- Andersen LH, et al. GlideScope videolaryngoscope vs. Macintosh direct laryngoscope for intubation of morbidly obese patients: a randomized trial. Acta Anaesthesiol Scand 2011; 55:1090.
- Ruetzler K, et al. McGrath Video Laryngoscope Versus Macintosh Direct Laryngoscopy for Intubation of Morbidly Obese Patients: A Randomized Trial. Anesth Analg 2020; 131:586.




