A 40 yo patient presents with a complaint of total arm paraesthesia and global loss of power. Over 16 hours previously she had a surgical procedure on her hand. A Brachial Plexus block (axillary approach), was used to provide anaesthesia. There has not been any return of function.
 On examination there is a total loss of sensation to the arm, loss of grip strength and a wrist drop.
On examination there is a total loss of sensation to the arm, loss of grip strength and a wrist drop.
Management of this patient?
 A rapid bedside ultrasound was performed that demonstrated a collection. A formal ultrasound then demonstrated a haematoma of 15mm x 140cm surrounding the axillary-brachial plexus complex.
A rapid bedside ultrasound was performed that demonstrated a collection. A formal ultrasound then demonstrated a haematoma of 15mm x 140cm surrounding the axillary-brachial plexus complex.
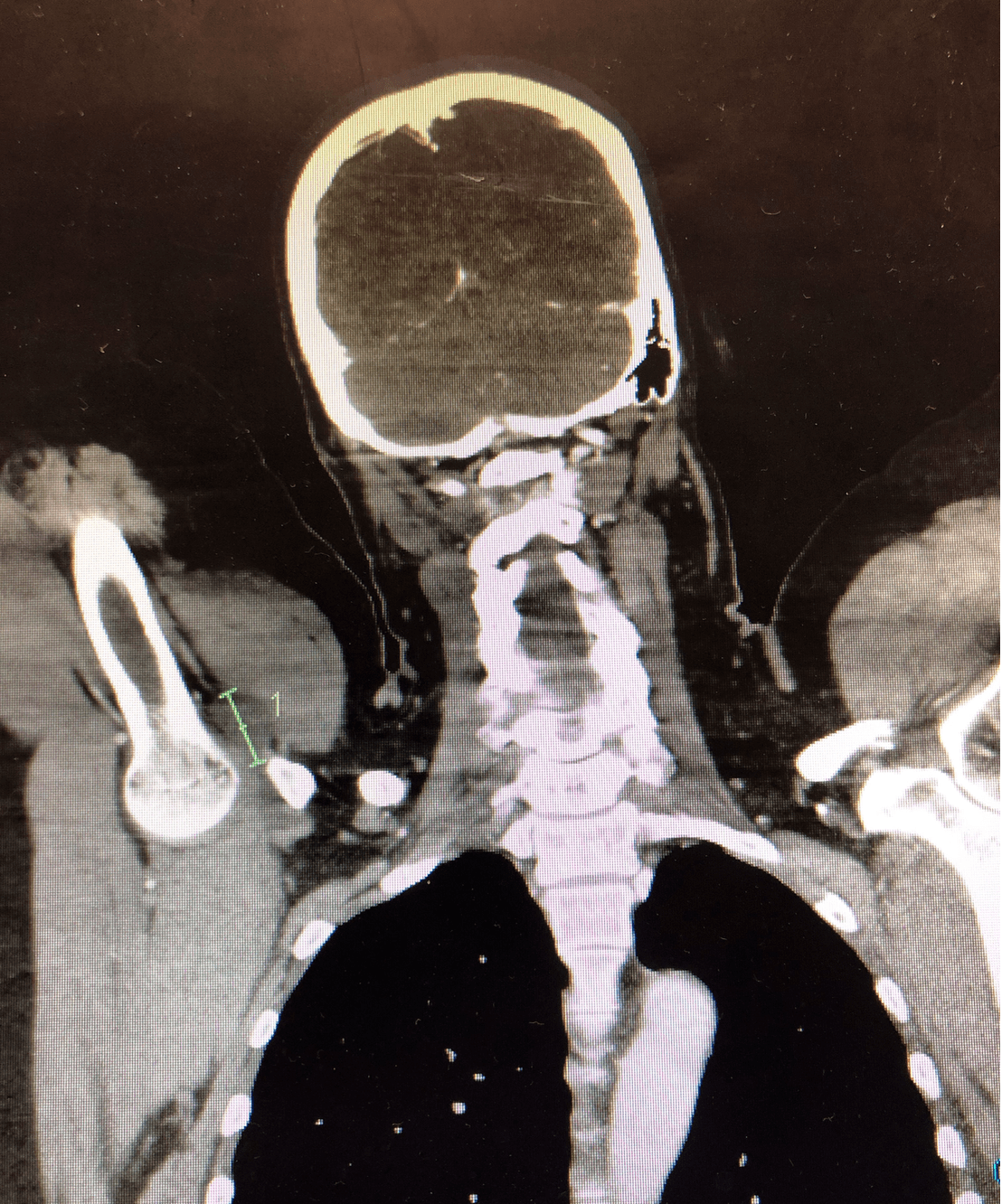
Given no MRI was available, a CT was performed by the surgical team that was not as clear. It potentially also showed some nerve oedema.
The patient was transferred to a Quaternary centre for combined vascular and neurosurgical operative intervention.
What is a Brachial Plexus Block?
It is a technique for establishing operative anaesthesia and pain relief of the upper limb.
There are three main approaches, each with a different potential complication.
- Interscalene approach: It is indicated for procedures on the shoulder and proximal humerus It can be used in surgery of the arm or forearm, however there is a high incidence of incomplete inferior trunk blockade, such that the ulnar distribution, is inadequately anaesthetised. It is associated with a higher incidence of dysfunction including potential injuries of the spinal cord and vertebral artery puncture.
- Supraclavicular approach: It may be associated with pneumothorax complications.
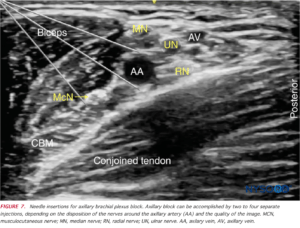
- Axillary approach: It involves deposition of local anaesthetic around the axillary artery, where three of the four major branches are located. It is used for lower limb anaesthesia.

Source: nysora.com
Complications of the axillary approach?
The complications of the interscalene and supraclavicular approach have been described above. The specific complications that can occur in the axillary approach are:
- Direct injury to the nerve: This is usually accompanied by pain which may be burning or shooting in nature
- Haematoma formation compressing the nerve: Symptoms of dysfunction may be delayed due to haematoma formation. Remember that the aim this approach is to infiltrate around the axillary artery adjacent to the axillary nerves. Although this is performed under ultrasound guidance, there is still the chance of puncturing a blood vessel.
Investigations
Here are some of the investigations that we can use to identify the potential injury.
- Electromyography: This is mostly used for direct nerve injuries ie nerve transection. It is not detectable early and is usually performed at 3-4 weeks post nerve damage
- MRI: It can identify an oedematous nerve or haematoma compressing the nerve
- Ultrasound: It can identify an oedamous nerve or a haematoma formation
- CT/CTA: If no MRI is available and there is a concern over a potential arterial injury, then a CTA may assist.
Management
- If there is neurological damage, with intact fascicles, then conservative management is indicated
- Haematoma requires rapid evacuation. It is shown and instinctively makes sense that earlier evacuation(<4 hours) is associated with a better prognosis
References
- Hyun J K et al. Brachial Plexus injury as a complication after nerve block or vessel puncture. Korean J Pain. 2014 27(3):210-218
- Woolley EJ et al. Neurological sequelae of brachial plexus nerve block. Ann Surg. 1959:149:53-60