The Pulse Check
During the rhythm check during CPR someone checked the pulse.
During the rhythm check someone checked the pulse.
Old ATLS teaching was it that a carotid or femoral pulse being present, meant that the systolic blood pressure was at least 70mmHg.
Studies have shown that our ability to detect a pulse and the accuracy of the reading are unreliable. Also the blood pressure with a pulse present can be less than 60mmHg
Deakin et al BMJ 2000 Sept 16;321(7262):673-674
CPR
CPR is everything and distinguishes between NO FLOW(no CPR) and LOW FLOW(CPR). At best we will achieve 50% of normal cardiac output (yes, that’s with the best CPR we can perform). It’s not great, but it again reinforces the need to continue CPR and not interrupt it.
The QUALITY OF CPR IS DEFINED BY:
- Chest compression FRACTION
- Chest compression RATE
- A quick word on RATE OF CPR:
100 compressions per minute is the recommended rate, however data from in-hospital cardiac arrests have shown that when the rate is too slow, return of spontaneous circulation(ROSC) falls from 72% to 42%
Animal models have shown that faster rates lead to better cardiac output.
A 2017 prospective observational study that measured ROSC in in-hospital cardiac arrests found that the greatest chance of ROSC was with a rate of 121-140. Resuscitation Jan 2017 Vol 110 pp154-161
- A quick word on RATE OF CPR:
- Chest compression DEPTH
- Chest RECOIL
Go to the Cardiac Arrest Pearls Section to find out more.
AIRWAY
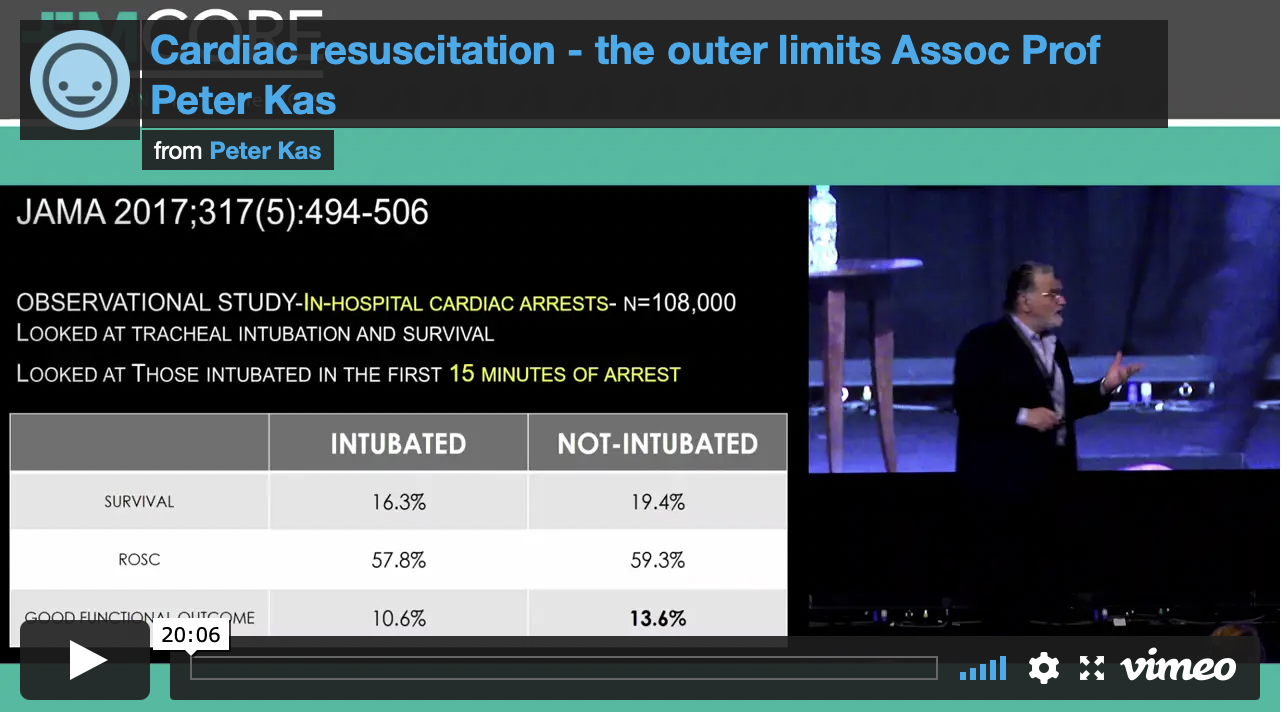
Everyone is obsessed with “getting the tube in”. In resuscitations, the airway is simple, unless there are compelling reasons to; do not intubate until ROSC is achieved. Intubation confers no benefit over supraglottic airway.
SOME POINTS ON AIRWAY
- We don’t know the best time to intubate
- It is difficult to intubate without interrupting CPR. This is an important point. If you have a video laryngoscope and can coordinate your intubation with CPR, then go ahead. However do NOT interrupt CPR to intubate
- Without adequate ETCO2, as occurs during cardiac arrest, it is difficult to very Ett placement.
- I BVM the patient and intubate only when ROSC is achieved.
All Patients should be intubated as soon as possible following a cardiac arrest: True/False?
The studies in out of hospital cardiac arrest showed that intubation conferred no benefit over BVM or supraglottic airway. In in-hospital cardiac arrests, those patients intubated within the first 15 minutes of cardiac arrest, had a worst outcome.
ADRENALINE
The use of 1 mg of adrenaline which initially came from canine models, was introduced at this time and has been a major part of all resuscitations since then.
The clinical significance of adrenaline is uncertain. It’s been shown to give no improvement and even to decrease survival to hospital discharge and decrease the rate of favourable neurological outcomes. Steil in the multi-centre OPALS study demonstrated no improvement in neurologically intact survivors to hospital discharge when using advanced life-support. We know that high-dose adrenaline doesn’t improve outcomes.
Jacobs, further randomised 601 cardiac arrest patients and found a significantly improved likelihood of achieving return of spontaneous circulation(ROSC) in the adrenaline group. There was a trend to increased survival to discharge in this group, unfortunately the study was underpowered.
Everyone should get 1mg of Adrenaline right?
Giving 1mg of adrenaline to a heart that has just resumed beating, can have dire consequences. The effect of markedly increased afterload against which a weak heart must beat, can result in a rapid loss of circulation. The adrenaline dose must be titrated to achieve adequate coronary and cerebral perfusion.
Our aim should be to achieve a coronary perfusion pressure of above 15 – 20 mmHg. This equates to diastolic blood pressure of 25 – 35 mmHg, which has been shown to provide adequate cerebral perfusion pressure.
Monitoring with an arterial line is the only way to do this accurately. As I have discussed at several EMCORE conferences, the aim is to locate the femoral artery with ultrasound during the first rhythm check pause and to then pass the catheter during the second rhythm check. This requires practice and coordination of the team.
If you don’t have an arterial line, don’t trust the pulse check, or the electrical wave form. Use the cardiac ultrasound to verify whether the heart is beating or not.
In the FEEL study it was found the 38% of patients with asystole on the ECG, had coordinated cardiac motion on echo. It was further found that 58% of those in PEA had coordinated cardiac motion seen when the heart was visualised. Hypothesize what might happen with the massive alpha effects of giving 1 mg of adrenaline to these hearts. Keep the dose small if the heart is beating.