The local GP calls you as the admitting officer of a rural emergency department and tells you he has a patient who has: Lower back pain, Numbness in both feet and Impotence
The GP has performed a CT this morning from L1 down, which was normal. You advise the GP that you think the diagnosis is cauda equina and the patient should go to the nearest major centre, but he arrives at your doorstep.
He is a 54 year old male with a history of lumber disc prolapse, for which he has had two previous laminectomies. As a result of this previous disc prolapse he has left leg weakness.
There is no other past medical history. The patient is not on any medications and has no allergies. On further history taking, he tells you that he has had these symptoms for several days. He feels that the symptoms have progressed and that both legs are now weak and numb, but there is no urinary or faecal incontinence.
Examination reveals the following:
-Decreased sensitivity to soft touch and pin-prick bilaterally
-Decreased power 3.7/5 bilaterally
-Decreased perianal sensation
-Sphincter tone intact
-Lower limb reflexes intact but depressed
What do you do now? What is the diagnosis?
We should all be thinking of cauda equina. Could it be conus medullaris syndrome instead of canda equina and does it matter if it is?
How do you differentiate medullaris from equina and what is it?
Can we predict how well this patient might do?
DISCUSSION
The most important thing to do for this patient is to get an urgent MRI. Even though the CT is normal, the MRI will give you much more detail.
This is not a diagnosis to miss, as it can result in longstanding complications. It is interesting to note that as soon as we scan the web, that there are legal firms out there specialising in cauda equina syndrome!!!
ANATOMY – briefly
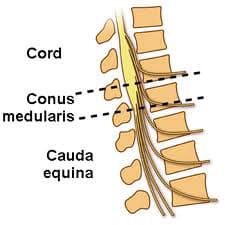 The spinal cord ends at the level of L1-L2. The distal part of the cord it the conus medullaris and its distal end continues as the filum terminalae. Distal to the conus, there are nerve roots and endings that look like a horse’s tail (thus the term canda equina). Cauda Equina Syndrome occurs when there is compression of the lumbosacral nerve roots.
The spinal cord ends at the level of L1-L2. The distal part of the cord it the conus medullaris and its distal end continues as the filum terminalae. Distal to the conus, there are nerve roots and endings that look like a horse’s tail (thus the term canda equina). Cauda Equina Syndrome occurs when there is compression of the lumbosacral nerve roots.
What causes compression of the cord?
- Central lumbar disc protrusion of L4/5 or L5S1
- Lumbar canal stenosis
- Trauma
- Tumours – metastases – lung, breast, renal
- Infection – abscess
- Haematoma
CLINICAL PRESENTATION
Patients can present with a pure canda equina or conus medalluris syndrome, or a mixture of both. Canda equina syndrome is really a peripheral nerve lesion. Conus medullaris Syndrome may have some upper motor neurone(UMN) signs and present with increased tone and reflexes (UMN) and bilateral signs. In terms of the Emergency Department diagnosis, differentiating between the two syndromes doesn’t matter, as the management is the same. What’s needed is an MRI and urgent referral.
Beware not to mistake the signs for a stroke, or miss a stroke.
What occurs clinically?
- Lower back pain– sciatica
- Power – decreased power in lower limbs – symmetrical or asymetrical
- Sensory – decreased sensation in lower limbs and saddle area to light touch / pin prick
- Reflexes – knee (spaned in conus) Ankle and Plantar reflexes affected.
- Erectile dysfunction
- Sphincter dysfunction -Urinary retention/Decrease urethral sensation/Loss of anal tone.
PROGNOSIS
Those with shorter time to treatment do better . Those patients with unilateral deficits do better (J. Bone Joint Surgery 1965). Recovery is proportional to the extent of saddle sensory deficit (Ann R. Coll Surg Engl 2008)
IN SUMMARY
Cauda Equina is a medical emergency.
If the patient presents with back pain and leg and perianal numbness, leg weakness as well as impotency and any urinary symptoms, get an MRI and refer to the spinal surgeons urgently.
Peter Kas





