In recent blogs I suggested that clinically significant C spine injuries can be excluded by CT scan in the intoxicated patient and Luke Lawton raised the suggestion that the hard collar may not be as efficacious as we were led to believe in our youth.
One of the questions that the C spine blog attracted was whether a femoral fracture would be considered a “significant distracting injury” and thus preclude clinical clearance of the C spine.
We are all taught in ATLS and EMST that a c-spine cannot be clinically cleared if there are painful distracting injuries present. This has been accepted dogma for some time and has been included in some of the decision rules around trauma assessment since.
If we consider the Nexus criteria for clinical clearance of the C spine (1)
Midline cervical tenderness
Present if pain is elicited on palpation of the posterior cervical midline from the nuchal ridge to the prominence of the first thoracic vertebra, or if pain is reported on palpation of any cervical spinous process
Altered mental status
- Glasgow Coma Scale ≤14
- Disorientation to time, place, person or events
- Inability to remember three objects at 5 minutes
- Delayed or inappropriate response to external stimuli
- Focal neurologic deficit
- Any patient-reported or examiner-elicited neurologic deficit
- Evidence of intoxication
- Recent history reported by the patient or an observer of intoxication or intoxicating ingestion
- Evidence of intoxication on physical examination, such as odour of alcohol, slurred speech, ataxia, dysmetria, or other cerebellar findings
- Behaviour consistent with intoxication
- Tests of bodily secretions are positive for drugs (including but not limited to alcohol) affecting mental alertness
Painful distracting injury
Any condition thought by the clinician to be producing pain sufficient to distract the patient from a cervical spine injury. Examples may include:
- any long bone fracture
- a significant visceral injury
- a large laceration, degloving injury, or crush injury
- extensive burns
- any other injury producing acute functional impairment
But as I alluded to in the intoxicated blog the question of what constitutes a significant distracting injury has not be further clarified and the suggestions above are just that, suggestions. And, in fact, does the presence of a distracting injury really mean that a competent patient, unimpaired by drugs or head injury, will fail to notice a clinically significant injury of their neck?
The same question was posed by the investigators in the 2001 first derivation of the Canadian C spine rules by Stiell et al. (2). That paper also noted that the NEXUS criteria “author’s own calculated specificity of 12% is very low and may actually lead to an increase in the use C-spine radiology in counties outside of the United States. Clinicians in Canada have found 2 of the criteria (“presence of intoxication” and “distracting painful injuries”) to be poorly reproducible”
A subsequent comparison paper (from the Canadian “Rules” group) demonstrated better specificity from NEXUS, but the rules did not perform as well as the Canadian ones. (3)
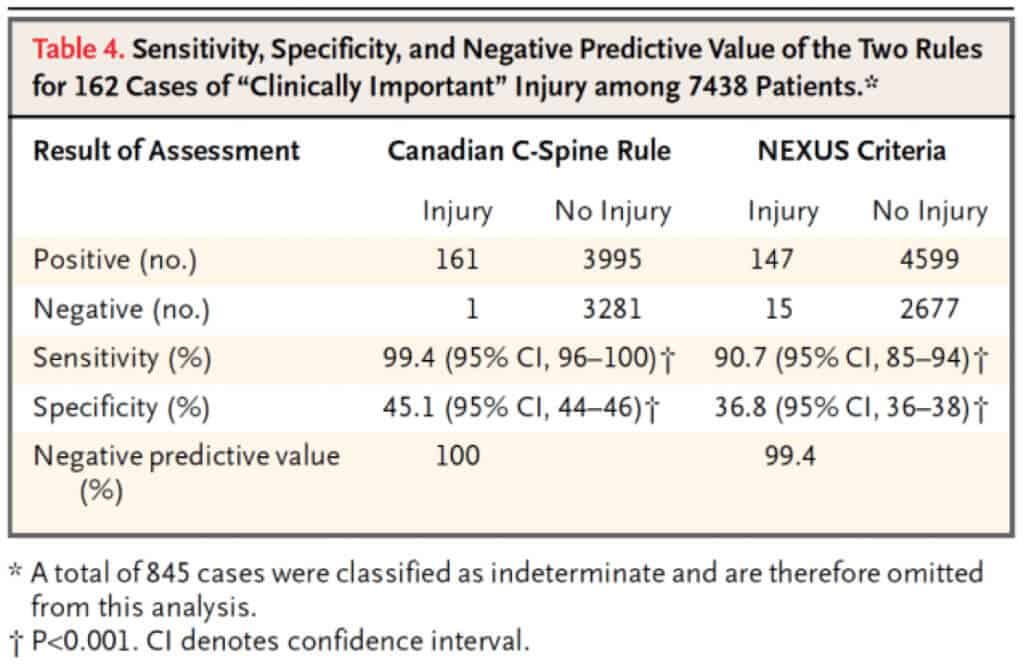
I will not go into the practical application of these decision tools; suffice it to say that I can never remember all the Canadian criteria despite them performing better. Thus we have 2 tools; one of which is a better tool that is harder to use and the other is a clumsy tool that is easy to apply. To improve things we either need an easier to use Canadian C-spine rule or more sensitive NEXUS criteria.
One of the things that leads to excess imaging in the NEXUS Criteria is the exclusion of those with distracting injuries from clearance by examination alone.
We discussed the sensitivity of helical CT in the clearance of the C-spine in a recent blog and if we accept that argument and consider the generally accepted sensitivity of C-spine CT is above 99% with a negative predictive value for clinically significant C-spine injury of 100%. (4,5) To be acceptable in the clinical situation the clinical examination needs to have a comparable sensitivity.
Several papers have been addressed the question of distracting injuries. Gonsalez et al prospectively studied 1439 blunt trauma patients with GCS 14 or 15. 897 patients were cleared by clinical examination and 442 had a positive examination and went on to have CT scans.. 134 had C-spine injuries on CT; 133 were noted on initial CT report with 1 missed. Follow up of the clinically cleared patients revealed 2 missed injuries- both were managed nonoperatively. A weakness of that study was patients with ‘‘distracting injuries’’ who were clinically cleared did not undergo definitive CT scanning of the c-spine to confirm that the negative clinical examination and follow up was clinical and then by phone call to elicit ongoing symptoms after discharge. Nevertheless both CT and clinical examination had a sensitivity of 99% irrespective of presence of distracting injury.
To address the shortcomings of the Gonsalez study another group embarked on a study of distracting injury effects on the sensitivity of clinical examination of blunt trauma patients with suspected C-spine injury.
“Clinical clearance of the cervical spine in patients with distracting injuries: It is time to dispel the myth” was published in The Journal of Trauma and Acute Care Surgery (7)
The group recruited 761 patients with blunt trauma and at least 1 distracting painful injury. Two-hundred ninety-six (39%) of the patients with ‘‘distracting injuries’’ had a positive c-spine clinical examination, 85 (29%) of whom were diagnosed with c-spine injury. Four hundred sixty-four (61%) of the patients with ‘‘distracting injuries’’ were initially clinically cleared, with one patient (0.2%) diagnosed with a c-spine injury. This yielded an overall sensitivity of 99% (85/86) and negative predictive value greater than 99% (463/464) for cervical spine clinical examination in awake and alert blunt trauma patients with ‘‘distracting injuries. The methodology was more rigorous with all patients irrespective of clinical findings being CT’ed.
The distracting injuries were not insignificant either; the list is below.
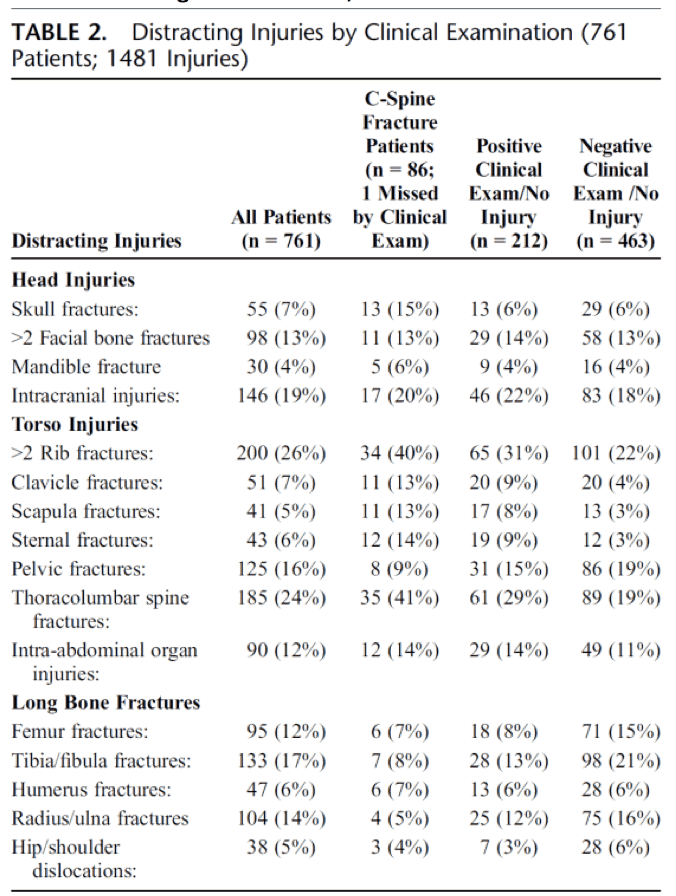
It should be noted that other authors have noted different sensitivities of clinical examination; Duane et al. found “Clinical examination cannot be relied upon to rule out c-spine fracture. CE is unreliable to diagnose or exclude a cervical spine fracture” Their group fo 534 patients had no distracting injury and no intoxication. There were 52 patients with, and 482 patients without, c-spine fractures. Forty of the 52 patients with fractures were accurately identified by clinical exam for a sensitivity of 76.9% and a NPV of 95.7%. In the group with an initial Glasgow Coma Score of 15, 16 of 24 patients with fractures were accurately identified for a sensitivity of 66.7% and an NPV of 96.5%. In the subset of patients who had no complaints of neck pain, external trauma of the c-spine or neurologic deficit, tenderness or abnormalities to palpation over the cervical spine would not require any radiographic evaluation There were 17 fractures and 10 were accurately identified by clinical examination. The sensitivity in this group was 58.8% with an NPV of 96.4%. Four of the seven missed injuries required intervention.
It should be noted that the clinical examination regimen described in the Rose paper was more rigorous than that employed by Duane et al. and is more rigorous than the one I would normally use. Rose et al included tenderness of the lateral neck whereas traditional assessments use midline cervical tenderness only. Maybe this is the key to the greater sensitivity, it effect on specificity has not been quantified.
The approach used in the rose trial is shown below.
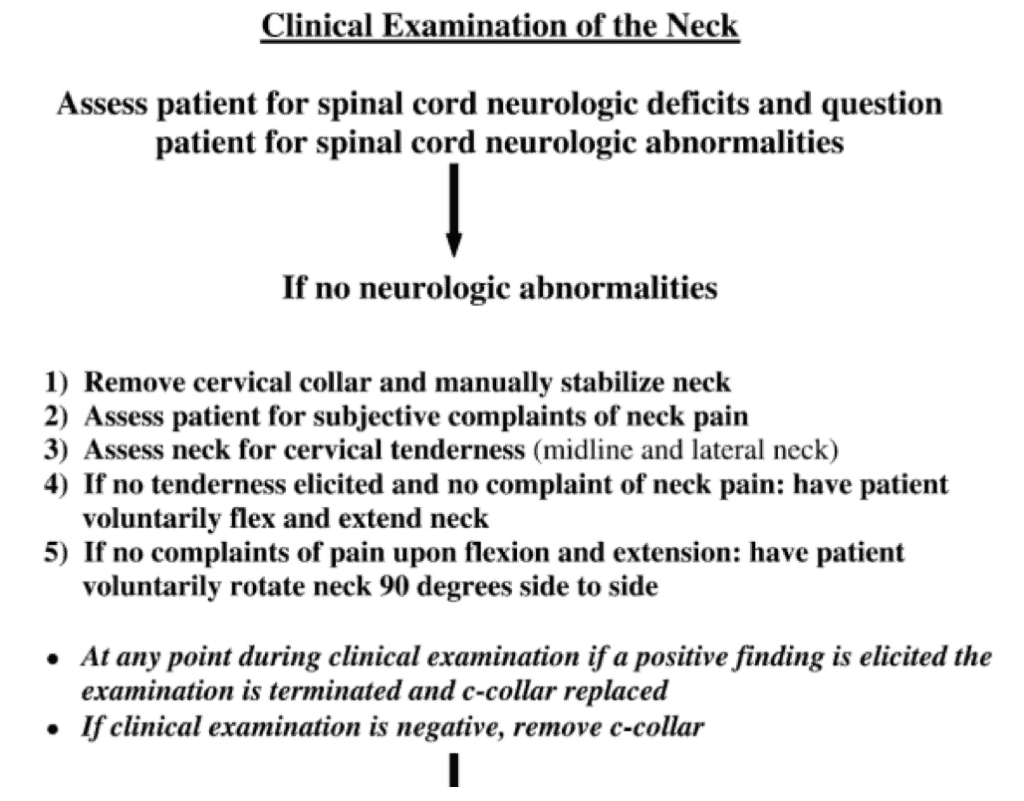
We are improving our tools for assessment of the C-spine of blunt trauma patients all the time. I am convinced that the clinical examination in conjunction with sensible CT scan use is the key to this and the days of mindless CT scanning of asymptomatic c-spine patients are numbered. We just need a better tool and the ability to use that tool. Perhaps we need to adjust our examination and do away with the distracting injury clause. The evidence is mounting, it is not conclusive yet, but is certainly something to think about.
References
- Panacek et al. Test performance of the individual NEXUS low-risk clinical screening criteria for cervical spine injury. Ann Emerg Med 2001;38:22–5
- Stiell IG et al. The Canadian C-Spine Rule for radiography in alert and stable trauma patients. JAMA 2001;286:1841-8.
- Stiell et al. The Canadian C-Spine Rule versus the NEXUS Low-Risk Criteria in Patients with Trauma N Engl J Med 2003 349;26
- Martin et al. Cervical spine evaluation and clearance in the intoxicated patient: A prospective Western Trauma Association Multi-Institutional Trial and Survey. J Trauma Acute Care Surg; 83,6: 1032-1040
- Brown et al. Spiral computed tomography for the initial evaluation of spine trauma: a new standard of care. J Trauma. 2006;61(12):382-387.
- Gonzalez et al. Clinical examination in complement with computed tomography scan: an effective method for identification of cervical spine injury. J Trauma. 2009;67:1297-1304.
- Rose et al. Clinical clearance of the cervical spine in patients with distracting injuries: It is time to dispel the myth. J Trauma Acute Care Surg 2012;73:498-502
- Duane et al. Clinical examination and its reliability in identifying cervical spine fractures. J Trauma. 2007;62:1405-1410.
 Dr Will Davies
Dr Will Davies