Here’s the case:
Here’s the case:
An 80 year old male is brought in by ambulance. GCS = 3, spontaneously breathing, laryngeal mask in place. Normally well man, past medical history of diabetes and hypertension. Following dinner that evening, his wife heard him call out. He said he couldn’t see and then lost consciousness.
According to the ambulance, when they arrived at the scene, he had a pulse rate of 90 bpm, was hypertensive at 200mmHg systolic and had a persistent GCS of 3. They placed a laryngeal mask and brought him into the department. In the department, a rapid examination revealed:
Vitals : PR 87bpm, BP 144/80, RR 12 bpm, GCS 3
Dual heart sounds. On chest auscultation, had crepitations in the right lung. There was no response to pain. The planters were upgoing bilaterally. The only other thing that I tested at this time was the Oculocephalic reflex i.e. dolls eyes. He had lost the reflex, so the working diagnosis was a brainstem infarct. Given his functional status, he was intubated with rapid sequence intubation and transfered to ICU.
CT head was normal. Further scanning in ICU demonstrated a basilar artery occlusion and resultant brainstem infarction.
What is the Occulocephalic Reflex?
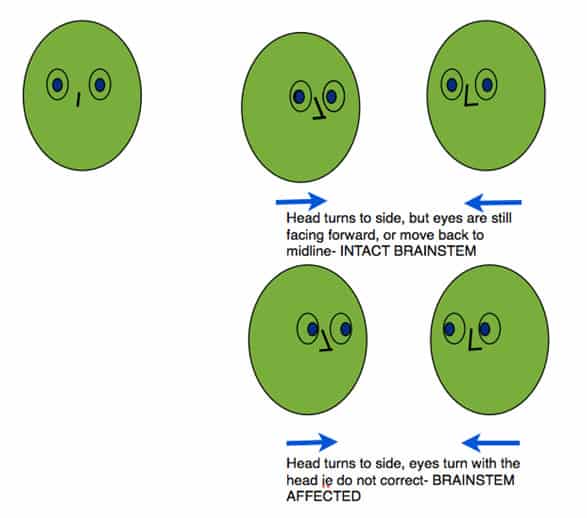
This really tests brainstem function. When the head is turned from side to side, the eyes should move in the direction opposite to the head turn, so they are looking ‘ forward’. A loss of this reflex results in the eyes being fixed and turning with the head and not moving back to the midline. This is a very useful test to assess brainstem function in the comatose patient. It obviously shouldn’t be done, if there is a risk of a cervical injury.
Something to try next time when the non-trauma, obtunded patient comes in.