The Case
A 58 yo patient presents to the emergency department with central crushing chest pain that came on abruptly and moved through to his back. The pain was rated as being 8/10. There was no shortness of breath, no diaphoresis and no vomiting.
The patient has not had chest pain previously, but does take medication for hypertension and is a smoker as well as having a family history of heart disease.
His vitals show a normal temperature, a heart rate of 92bpm and a BP of 140/68. There is no major difference in blood pressure between the arms and there is no pulse deficit. Heart sounds are dual with no added heart sounds and the abdomen is soft. Rapid Neurological examination is normal.
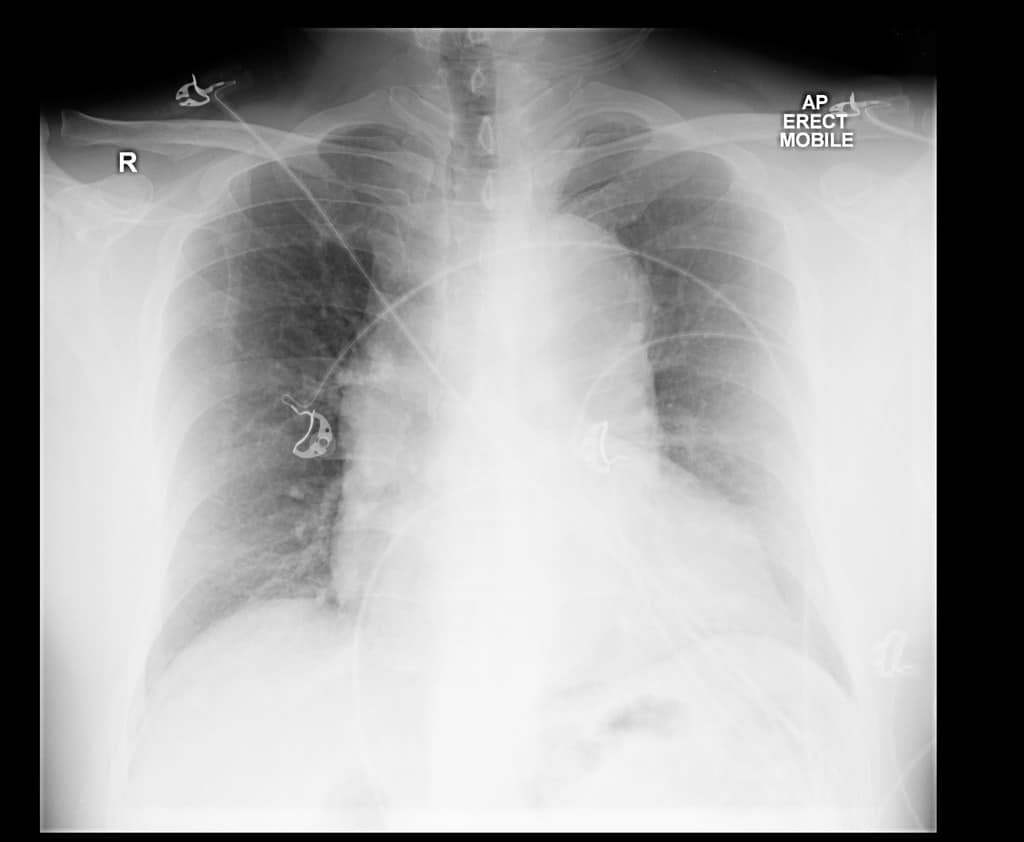
An ECG is done, with no ischaemic or other changes. The patient’s chest x-ray is shown below, and was considered normal.
300mg of Aspirin is given, as well as 2 x 25 mcg of Fentanyl IV, after which the patient’s pain is reduced to a 3/10. Further fentanyl is given, however it is difficult to receive the pain totally. An initial high sensitivity troponin is negative as is the repeat troponin, 3 hours later. The pain-free ECG is also normal.
The registrar asks “Could it be a dissection?” “Should I do a D-Dimer?” The resident adds “It can’t be a dissection, if the chest x-ray is normal…can it?”.
Thoracic Aortic Dissection
Thoracic Aortic Dissection has been called the great mimic. It is the one condition where the art of medicine is still alive and well. Recently there have been some good studies that give us the tools to risk stratify patients with suspect thoracic aortic dissection and to even consider low risk rule outs using a D-Dimer(beware here as these studies have not been externally validated). What we really need is a decision rule that identifies patients as no risk.
Try the following questions:
What is the sensitivity of Chest-Xray for thoracic aortic dissection?
Perhaps a better question is what percentage of patients with aortic dissection have a widened mediastinum? Or can we rule our aortic dissection with a normal chest x-ray?
Only 62% of patients with dissection have a widened mediastinum
Look for a mediastinum width > 8cm on anteroposterior(AP) view.
We cannot rule out a dissection if the chest x-ray is normal..
What else can cause a widened mediastinum?
- A tortuous aorta may look like aortic dissection. This can occur in hypertensive patients.
- Tumour
- Lymphoma
- Thyroid enlargement
History
Order these pain characteristics from highest to lowest in terms of predicting a thoracic aortic dissection.
-Sudden Onset Pain
-Tearing/Ripping Pain
-Migratory Pain
- Tearing/Ripping Pain (LR 11)
- Migratory Pain (LR 8)
- Sudden Onset Pain (LR 3)
What percentage of patients have painless Thoracic Aortic Dissection?
1 in 20 (5%) will have a painless thoracic aortic dissection……..Good luck.
Examination
Which of these three examination findings in a suspected Thoracic Aortic Dissection has the highest likelihood ratio for predicting a dissection?
-Pulse Deficit?
-Diastolic Murmur?
-Focal Neurological Finding?
- Focal Neurological Deficit (LR 33)
- Diastolic Murmur (LR 5)
- Pulse Deficit (LR 3)
Chest Pain PLUS Criteria
As in syncope where we have the Syncope PLUS criteria, in suspected aortic dissection, we must think of the Chest Pain PLUS Criteria.
- Chest Pain PLUS SYNCOPE = Dissection or acute ischaemia
- Chest Pain PLUS NEUROLOGY = Dissection: Dissection can extend into the carotids or downward and affect the spinal cord.
- Chest Pain PLUS PAIN or SYMPTOMS above and below the diaphragm = Dissection
Risk Stratification of patients with suspected Thoracic Aortic Dissection
The aortic dissection detection risk score ADD-RS has a high sensitivity for picking diagnosing thoracic aortic dissection, with only the information available at the bedside. You can score one point from each of these three areas.
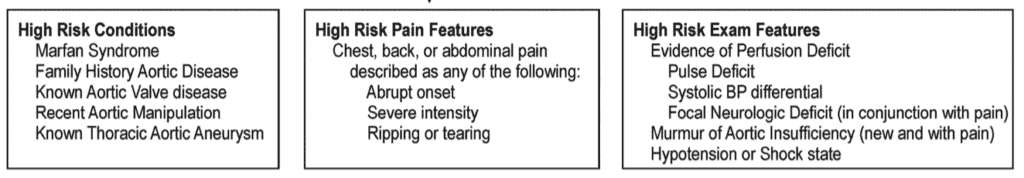
0 is low risk
1 is intermediate risk
2-3 is high risk.
Our 58 yo patient with abrupt onset of pain and a history of hypertension and smoking, scores:
High Risk Conditions: 0
High Risk Pain Features: 1
High Risk Exam Features: 0
Can we use D-dimer to decide if imaging is needed?
CTA is the investigation of choice, although MRA and TOE can be used. Point of care ultrasound may rule in a dissection, but at this point cannot rule out a dissection.
The ADvISED Trial looked at using D-Dimer to rule out Aortic Dissection in low risk patients.
What they did
Multicenter prospective observational trial
Used the Aortic Dissection Detection Risk Score with a D-Dimer to exclude dissection.
n= 1850
Their Conclusions were:
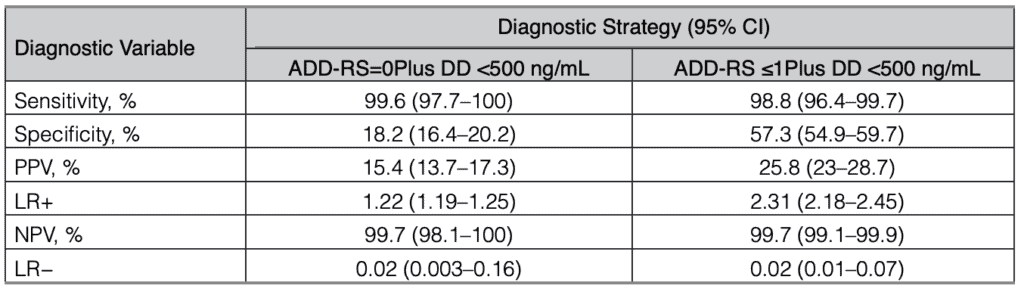
This table tells us that an ADD-RS score of 0 or 1 and a D-Dimer of < 500ng/mL has a 99.7 NEGATIVE PREDICTIVE VALUE for a Thoracic Aortic Dissection. Remember that predictive values are dependant on the prevalence of the disease in the population.
The proposed approach in this study is shown below.
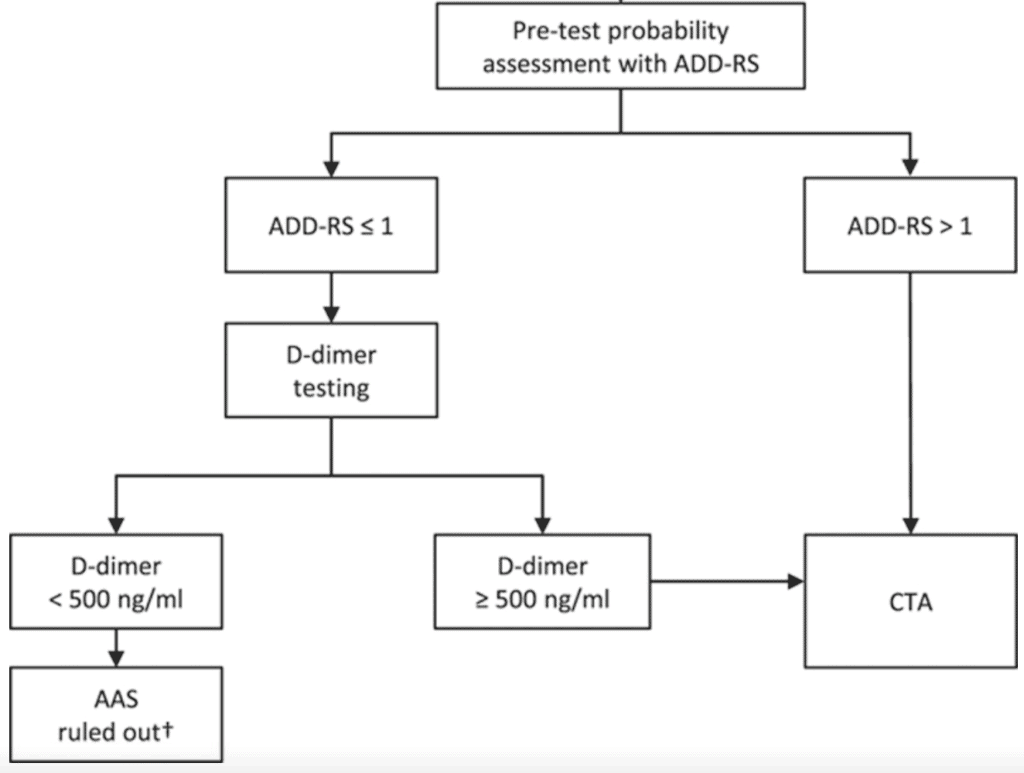
Let’s return to our 58 yo patient above with a past history of hypertension and smoking who presents with a rapid onset of chest pain. He would score a 1 on the ADD-RS. We could potentially rule him out with a normal D-Dimer.
We need to be aware of a few things in this study:
- It has not been externally validated as yet, so we need to take care when applying their findings.
- The miss rate with low risk score of 0 and a negative D-dimer was 1 in 300 cases.
- The use of the tool would avoid about one in two aortograms
Would I use it?
With great care due to the lack of external validation. It needs to be used in the right population. It may be a shared decision making exercise. I don’t know that I have seen more than 10 or so dissections in my career, so missing 1 in 300 may not be such a large number.
What would be the benefit of using it?
- Decrease the number or aortograms done. However the number is so small that it really doesn’t affect us from a volume point of view.
- Risk of contrast induced nephropathy? We have already seen the studies which show that this is not a big issue.
I’m not sure that there is a great downside in occasionally having to do an aortogram ie., one every few months. If the volume is larger, then it may be of benefit.
References
- Nazerian P et al. Diagnostic Accuracy of the Aortic Dissection Detection Risk Score Plus D-Dimer for Acute Aortic Syndromes. Circulation Volume 137, Issue 3, 16 January 2018; Pages 250-258
- Rogers A et al. Sensitivity of the Aortic Dissection Detection Risk Score, a Novel Guideline-Based Tool for Identification of Acute Aortic Dissection at Initial Presentation. Circulation Volume 123, Issue 20, 24 May 2011; Pages 2213-2218