Massive propranolol overdose is perhaps one of the most challenging overdoses to manage. In 2009 we posted a case we had. We have progressed in our management since then.
CASE
A 26 yo woman is brought to the ED by ambulance. She has been found by her mother in her bedroom in a confused state. She had been seen 45 minutes earlier and had been well. The ambulance report that there are 60 x 40mg tablets of Propranolol that are missing.
On arrival the ambulance officers state that the patients GCS was 13 and blood glucose was 5.5. The ambulance have established intravenous access, but given nothing.
On arrival the patient’s GCS is 9-10 and within 5 minutes of arrival the patient has a generalised tonic clonic seizure lasting less than 30 seconds.
On arrival the patients vitals are as follows:
HR 60 bpm
BP 105/40 mmHg
Sats 98% on 6L
RR 20
What can we say so far?
Haemodynamically the patient is holder her own. Why are her sats only 98% on 6L of oxygen and her respiratory rate is high? Has she aspirated?
What should we be thinking about interns of the drug taken, the amount taken and the time it was taken?
Propranolol is considered one of the most toxic, non-cardiac selective beta blockers available. It can affect beta 1 and beta 2 receptors causing bradycardia and hypotension. It also has membrane stabilising ability blocking myocyte Na channels and can therefore prolong QRS duration and affect cardiac conduction.
It has high lipid solubility allowing it to rapidly enter the central nervous system and its high protein binding make it difficult to dialyse. It is hepatically metabolised and excreted in the urine.
It’s absorption is rapid with many signs developing within 30 minutes and most signs usually present within 60 minutes. All patients have symptoms within 6 hours.
A dose greater than 1g is considered potentially lethal.
What are some of the signs and symptoms you might expect to see?
In propranolol overdoses we have to deal with the beta blocker effects and the Na channel blocking effects.
Beta Blocker Effects
- Bradycardia: ranging from sinus to atrioventricular blocks
- Hypotension: secondary to decreased heart rate and decreased myocardial contractility.
- Bronchospasm
- Hyperkalaemia
- Hyper/Hypoglycaemia
Na Channel Blockade
- QRS widening and arrhythmias associated with this
- Seizures
- Confusion
- Coma
The Nurse hands you this ECG. What findings in this ECG may reflect the overdose and are they predictive in any way?
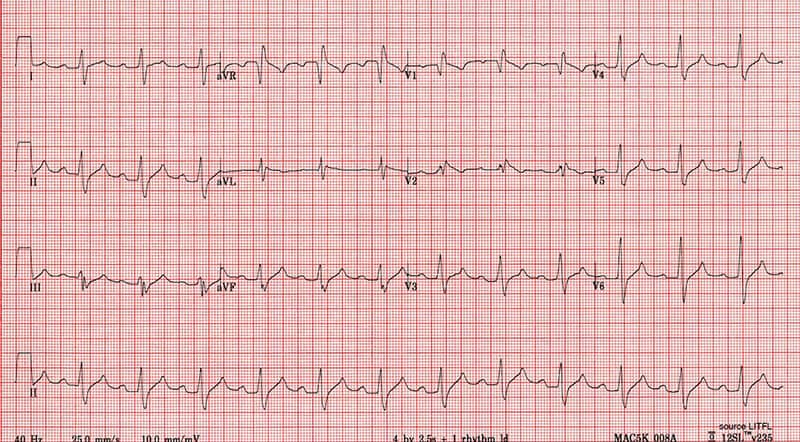
- Prolonged PR interval
- Right axis
- R wave in aVR > 3mm
The width of the QRS is predictive of seizures or arrhythmias, however it is not wide enough in this ECG.
ECG Changes that occur and what may be predictive
- Prolonged PR
- AVN blocks
- Sinus bradycardia
- Wide QRS: As in tricyclic overdose, this is predictive.
- QRS> 100ms: risk of seizures
- QRS> 160ms: Risk of Arrhythmias.
- Rightward axis
- Terminal R wave > 3mm in aVR
What are the priorities in this patient?
- Protect the airway
- The patient will need intubation. Lets use something that won’t drop the blood pressure any further ie Ketamine and Rocuronium. I would at this point give 1L of crystalloid to the patient whilst doing this.
- Hyperventilate the patient to a pH of 7.5
- Improve the haemodynamics
- This is where we have to decide on chronotropes, inotropes and sodium bicarbonate. read on for the possibilities.
Let’s compare this to a tricyclic overdose ECG shown below and we see a similarity, especially in the R wave in aVR. Why is this? This may give clues as to some similarity in treatment.
The patient’s haemodynamic status changes.
Vitals are:
HR 45bpm
BP 80/50 mmHg.
Briefly outline treatment strategies possible for stabilising this patient.
Initial rapid stabilisation is required. If the patient is in cardiac arrest, ACLS arrest protocols should be followed.
Seizures should be treated with benzodiazepines ie midazolam 0.15mg/kg
Arrhythmias should be treated with sodium bicarbonate(NaHCO3). Avoid Procainaimide, Amiodarone or Flecainide, as the sodium channels are already poisoned.
In early presentations and large ingestions, in patients with a normal conscious state, there is a place for charcoal.
In patients that require intubation, due to a depressed conscious state aim for ventilation to result in a pH 7.5-7.55
Na Channel Blockade
The widened QRS and terminal R wave in AVR should be treated as per tricyclics with NaHCO3. 1-2mmol/kg every 2 minutes until QRS normalises.
Beta Blocker Effects
There are a range of treatments and a progression through them, to deal with the beta effects, especially unstable haemodynamics. The range of treatments includes both chronotropes and inotropes. We start with the basics and quickly escalate, as in most cases the basic measures don’t work.
- Crystalloid: A fluid challenge with NaSaline 0.9% 10-20mL/kg
- Atropine: 10-30mcg/kg, to a maximum of 3g. This is a temporising measure and in most cases will not work.
- Glucagon: Still appears in some texts as first line management. 5mg IV bolus over 1 minute , then repeat in 5-10 minutes, then consider an infusion. This can even be used as a diagnostic challenge. However, in reality, it doesn’t work, as in most cases the hospitals have inadequate stock of this medications
- Isoprenaline: Need to increase the dose accordingly to achieve an effective blood pressure.
- Adrenaline: This can work as an inotrope and chronotrope, but find it doesnt work as well.
- High Dose Insulin Therapy:This provides good inotropic support, however there may be up to a 30 minute delay before it begins to work. Give 50mL of 50%(25g) glucose and 1IU/kg bolus, this is then followed by an infusion of 25g glucose and titrate to a BSL of 5-14mmol/L. Add short acting insulin at 0.5IU/kg/hr(max 5IU/kg/hr)
- Intralipid (Lipid Emulsion): It’s role is not clearly defined. It acts as a ‘lipid sink’ for fat soluble drugs removing them from target organs. It does have some potential adverse effects including acute kidney injury, venous thromboembolism and pancreatitis. It can be used in cardiac arrest that is refractory to other measures. Use 100ml of 20% IVLE(1-1.5mlkg) IV bolus and repeat at 3-5 minute intervals.
- Cardiac pacing:This is only used when medications are failing. It frequently fails to capture. Sometimes it will capture and it will increase the heart rate with no increase in perfusion.
- Haemodialysis: Propranolol is not removed by hemodialysis.
What would my approach be?
In any patient that presents early with a significant ingestion:
- Charcoal 50g PO
- Any QRS changes on the ECG give 1 – 2mmol/kg NaHCO3 every 2 minutes, until the QRS normalises.
- NSaline 1L fluid challenge
- Atropine 1g IV x 3(whilst adrenaline is getting ready)
- Adrenaline infusion as per cardiac protocol.
- High Dose insulin therapy
Let’s Compare this with something similar:
A 23 year old woman is brought to the emergency department with a depressed conscious state. She is believed to have taken an overdose, but of unknown substance. She was seen one hour prior to being found by her mother in an altered conscious state.
There is no evidence of trauma, and a past medical history of depression.
On arrivals the patients vitals are:
GCS 13
HR 122bpm
BP 98/57 mmHg
Sats 92% on room air.
The patient’s ECG is handed to you:
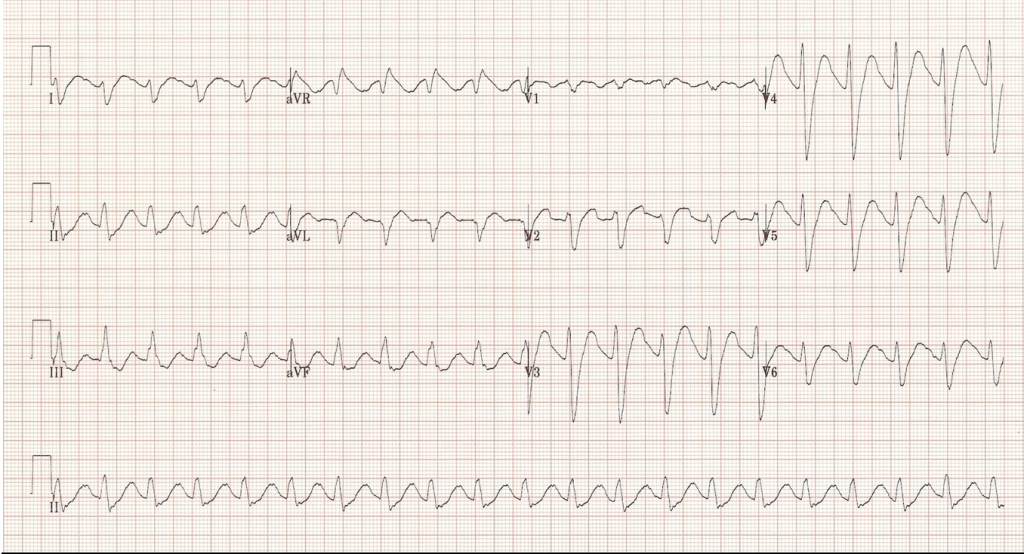
Source LITFL
The rate is about 126bpm. So its not likely to be a Beta blocker, however the Na channel blockage changes are present in aVR, with a terminal R wave. This is a tricyclic overdose.
Notice the Na channel blockage and the need to treat this patient with NaHCO3. In fact this is the main treatment.
The QRS duration is again predictive ie., >100ms is predictive of seizures and >160ms is predictive of arrhythmias.
Prior to any management strategies the patient becomes unresponsive and pulseless. The rhythm strip shows the following. You commence CPR and ACLS measures and your registrar intubates the patient ‘cold’.
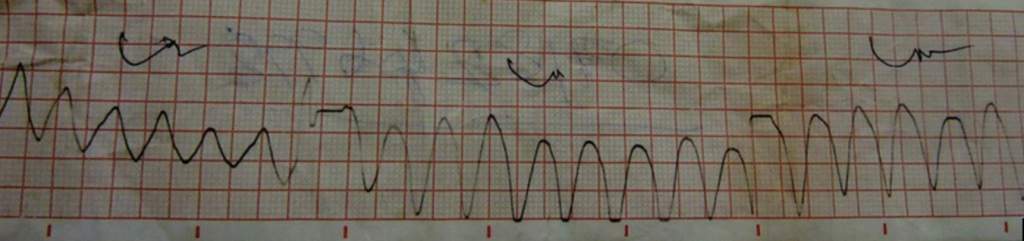 What drug do you avoid giving here?
What drug do you avoid giving here?
Amiodarone: It has Na channel blocking strategies and will poison already poisoned Na channels.
Peter Kas
See Associate Professor Peter Kas speak at the EMCORE Conferences.
Emergency Physician, Architect, Creator of resus.com.au, the EMCORE Conferences and ‘Own the ECG’




