Pulseless Electrical Activity(PEA) occurs in about 30% of cardiac arrest cases. Given that it’s not a shockable rhythm, it has a very poor prognosis, especially when associated with acute myocardial Infarction(MI)(1). More recently, the term pseudo-PEA, is used for those patients where we can’t find an output by feeling for a pulse, but there may in fact be one, when we view the heart by echocardiography. More on this will follow in the next few blogs.
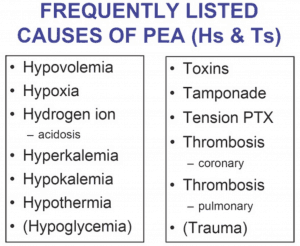
When confronted by the PEA patient, ACLS guidelines require us to quickly evaluate the potential cause by citing the H’s and T’s. I don’t know about you but I see people trying to think of them during an arrest and having trouble. In fact the literature shows that it is difficult during an arrest to remember them all(2), so you and I are not alone.
I personally have an approach that is as follows:
- Maximise oxygenation
- Give them fluid
- Could they be having a PE or MI or is there a cardiac tamponade?
- What’s their potassium doing?
- …..Then I’ve got to think of the others……..
That’s been my approach since I can remember.
Things have changed since these guidelines were produced. We now use echocardiography and certainly our appreciation of electrocardiographic tracings has much improved, yet neither ECG tracings nor echocardiography appear anywhere in these protocols.
In a 2014 paper, Littmann et al(3) proposed a new tool that simplified the approach to PEA by simply looking at the width of the QRS complex and dividing the causes based on QRS width.
- QRS duration < 0.12s (3 small squares)
- QRS duration > or = 0.12s
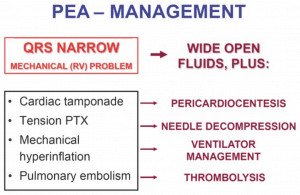
Narrow QRS <0.12s
This is usually caused by a mechanical problem due to an outflow obstruction.
The 4 most common causes are:
- Cardiac Tamponade
- Pulmonary Embolism
- Tension Pneumothorax
- Mechanical Hyperinflation
Using our bedside ultrasound we can look for the following:
- Collapsed right ventricle which indicates an obstruction to blood going to the heart and caused by:
- Tamponade
- Hyperinflation
- Pneumothorax
- Dilated Right Ventricle
- Pulmonary Embolism
Wide QRS > or = 0.12s
This is usually due to a metabolic problem or ischaemia and heart failure. This may be:
- Hyperkalaemia
- Sodium Channel Blocker Toxicity
- Cardiac Ischaemia
This approach doesn’t take into account hyperaemia, hypokalaemia, or hypoglycaemia, however the frequency of progression to PEA of these patients is very rare(4). The proposed approach doesn’t specifically use hypothermia or toxins but assumes that given the history of presentation, that these causes will be picked up.
How To Use This Approach
 In A Narrow QRS Complex PEA
In A Narrow QRS Complex PEA
- Start Fluid- Normal Saline and be aggressive as these causes may respond to fluid.
The echocardiogram can give the rest of the solution
- If there is PE: Thrombolytics
- If there is over ventilation, disconnect
- If a Tension pneumothorax then decompress.
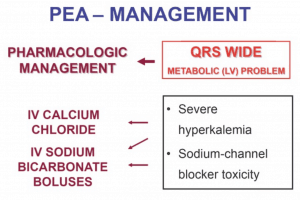
If A Wide QRS Complex PEA
- If Hyperkalaemia is suspected give NaHCO3 and Calcium
- If Na channel blockade is suspected, give NaHCO3
In Summary:
Please remember that this system is an academic proposal and as the author himself writes, there are some limitations, especially with patients with a pre-existing left bundle branch block or a massive PE, where the complexes may appear wide.
I like the approach because it makes me think differently and takes into account the very thing we are looking at throughout this whole scenario…the ECG trace.
References
- Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57.
- Morgan R, Westmoreland C. Survey of junior hospital doctors’ attitudes to cardiopulmonary resuscitation. Postgrad Med J. 2002;78:413–415.
- Littmann L, Bustin DJ, Haley MW. A Simplified and Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity. Med Princ Pract 2014;23:1-6.
- Desbiens NA. Simplifying the diagnosis and management of pulseless electrical activity in adults: a qualitative review. Crit Care Med. 2008;36:391–396.
Associate Professor Peter Kas


 In A Narrow QRS Complex PEA
In A Narrow QRS Complex PEA

