CASE
A 28 yo woman presents to the emergency department with chest pain and dyspnoea. She has been moving house and moved a heavy cabinet. The pain started soon after this.
She is normally healthy and has no risk factors for heart disease.
Her ECG is shown below.
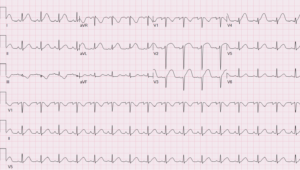
Image similar to this case from Viray M et al. JACC July 21st 1917
The ECG shows ST elevation in the infero-lateral leads with some reciprocal ST depression in the inferior leads.
CXR is normal and the Troponin is raised.
The patient is commenced on Aspirin and is given Heparin. Cardiology decide that a cardiac angiogram is needed. This shows a spontaneous coronary artery dissection(SCAD).
What is SCAD?
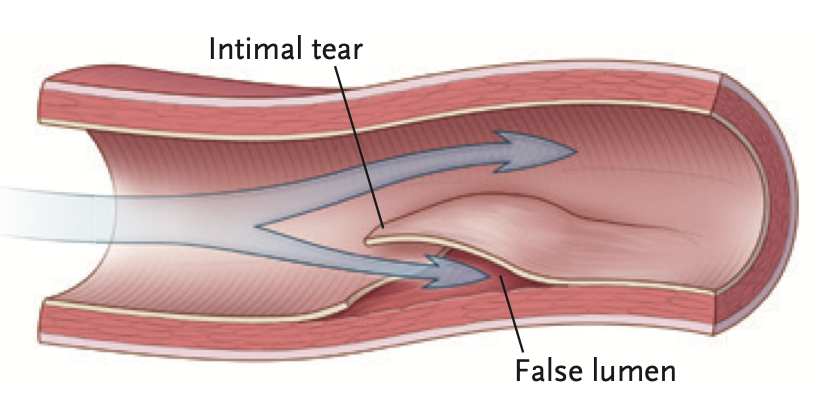
SCAD is a separation of layers of the coronary artery wall, resulting in intramural haemorrhage and haematoma formation. Coronary insufficiency results due to the narrowing of the coronary artery lumen, from an expanding intramural hameatoma. SCAD may or may not involve an intimal layer tear.

Source: NEJM 2020;383;24:pp 2358 – 2370 Type 1 SCAD has the pathognomonic angiographic appearance of an arterial dissection. On the right, optical coherence tomography (OCT), shows an intimal tear. Double-headed arrows show the intramural haematoma.
How Common is SCAD?
SCAD plays a prominent role in myocardial infarction in women. In total the disease accounts for approximately 1% of all acute myocardial infarctions. However 90% of cases of SCAD occurs in female patients between the ages of 47 and 53. It accounts for up to 20% of myocardial infarctions during pregnancy and is now increasingly being reported in older women.
Although the condition does occur in males, its prevalence is very low.
What are the Predisposing factors?
- Female sex hormones (10%) (this may oalso occur in patients that are trans-gender or on gender affirming hormones)
- Connective tissue diseases ie., Marfan, Ehler Danlos
- Fibromuscular Dysplasia (50%) The same genetic locus is associated with cervical artery dissection and migraines.
- Pregnancy (5%) mostly third trimester or early post partum.
- Factors that increase haemodynamic stress eg., Valsalva manoeuvres, vomiting, lifting
Making the diagnosis
Patients will present with typical ACS symptoms of chest pain(>90%), neck or back pain, dyspnoea, vomiting or diaphoresis. They will have ischaemic ECG changes and raised cardiac markers. Although a quarter of patients will have normal initial troponin levels, a significant number will have myocardial infarction and up to 50% will present with a STEMI. A smaller number (5%) present with ventricular arrhythmias.
It is important to consider the diagnosis in younger female patients presenting with chest pain and few or no cardiac risk factors, especially if there are associated precipitating factors.
It is especially important to consider the diagnosis in those situations where coronary angiography is not readily available and thrombolysis is the only treatment option available in acute myocardial infarction. Thrombolysis in SCAD, could prove to be catastrophic.
The diagnosis is generally made during angiography, as there are specific angiographic categories identified. In cases where this is difficult, the use of intravascular ultrasound or optical coherence tomography(OCT) can make the diagnosis.Intravascular and intracoronary imaging are associated with risks however. Coronary computed tomographic angiography(CCTA) can also be used, although this has limitations and can result in false positives.
Management
This is usually conservative as the lesions have shown to heal spontaneously. PCI is also a very challenging procedure in this condition. If there is ongoing infarction, percutaneous coronary intervention and even bypass grafting may be necessary.
Patients with high risk features require revascularisation.
High risk features include:
- Ongoing chest pain and evidence of ongoing ischaemia
- Shock
- Ventricular arrhythmias
- Multivessel involvement on angiogram
- Reduced TIMI flow
Dual anti-platelet therapy is used in those patients receiving a stent and may be continued (consensus opinion). Single anti-platelet therapy may be continued following the initial event, especially for patients with fibromuscular dysplasia, as Aspirin can prevent thrombosis.
Anticoagulation should not be used in confirmed SCAD.
Thrombolysis should be avoided as it is associated with deterioration in patients with SCAD.
Beta blockers can be used as per usual ACS guidelines. They may prevent recurrence of SCAD.
Statins are not usually needed as the disease is not related to an atherosclerotic plaque.
Nearly 20% of patients may present with a recurrence of SCAD, which is defined as a new dissection event different to the previous myocardial infarction, within the first week or so of initial presentation.
References
- Hayes SN, et al. American Heart Association Council on Peripheral Vascular Disease; Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Genomic and Precision Medicine; and Stroke Council. Spontaneous Coronary Artery Dissection: Current State of the Science: A Scientific Statement From the American Heart Association. Circulation. 2018 May 08;137(19):e523-e557.
- Hayes S et al. Spontaneous Coronary Artery Dissection. J Am Coll Card 2020 Aug 25;76(8): 961-984.
- Viray M et al. Pregnancy-associated spontaneous Coronary Artery Dissection in a young Prepartum female patient. J Am Coll Card July 21 1917.
- Alfonso F, Paulo M, Gonzalo N, et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomogra- phy. J Am Coll Cardiol 2012;59:1073-9.
- Kim E S H. et al., Spontaneous Coronary-Artery Dissection. NEJM 383;24 December 10 2020: pp 2358-2370.