Convulsive Status Epilepticus accounts for up to 75% of all status epilepticus(1). We recognise it in patients where they have a depressed conscious state accompanied by tonic clonic movements of the extremities. The length of status epilepticus is important in terms of patient survival. About 5% of adults and up to 25% of children with epilepsy will have at least one episode of status epilepticus.
Definitions
Status Epilepticus: The definition has changed over the years. Currently it is defined as any seizure lasting longer than 5 minutes, without a return to normal consciousness, or recurrent seizures without a return to normal consciousness between seizures.
Established Status Epilepticus is a seizure that continues following administration of first line medications such as benzodiazepines
Refractory Status Epilepticus is a seizure that doesn’t resolve following administration of benzodiazepines and anticonvulsants.(2)
Super Refractory Status Epilepticus is drug resistant status that either persists or recurs despite continuous intravenous anaesthetics for more than 24 hours.(3)
The times of 5 minutes and 30 minutes are important landmarks. Most seizures last less than 5 minutes. Those that don’t, don’t tend to stop spontaneously(4). A seizure lasting more than 30 minutes is associated with up to 19% mortality(5), and those with refractory status epilepticus have a mortality as high as 60%(6). The 30 minute landmark, where neuronal damage is believed to occur and pharmaco-resistance develops, is controversial and it is now believed that these things occur much earlier(7).
Receptors May Explain It
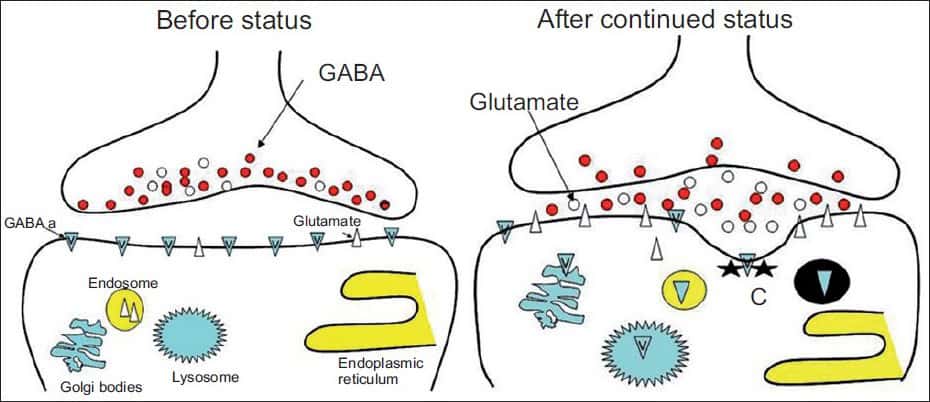
Most of the medications we use for the treatment of seizures, including midazolam, valproic acid, propofol, act on GABA receptors. It appears that during prolonged seizures, the number of activated GABA-A receptors on the postsynaptic membrane gradually decreases as they are internalised(8). However, glutamate-sensitive N-methyl-D-aspartate (NMDA) receptors significantly increase(9).
It would therefore make sense that the earlier a seizure is treated, the better the potential control of that seizure and thus the outcome.
How to best manage status epilepticus
Management of the seizure itself is very important however we must also think about why the seizure is occurring. In some of these cases pre-hospital personnel may give some clues, however for the most part we need to have a list for ourselves. I like to think of it as follows:
- In all patients I think of:
- Hypoglycaemia
- Hyponatraemia
- CNS infection
- Trauma
- Intracranial pathology: trauma or mass or bleed or stroke
- Drug toxicity/withdrawal
- In patient with known epilepsy
- Compliance: over/non
- Other medications that may compete with anti epileptics
- In young women that may be pregnant
- Eclampsia
First Line Treatment
Perhaps the best approach in the pre-hospital environment, or if the patient has a seizure in hospital is the rapid delivery of Benzodiazepines.
MIDAZOLAM
In adults my first choice would be MIDAZOLAM. If there is no intravenous access, it can be given intramuscularly at a dose of 0.15mg/kg, or a standard adult dose of 10mg IM. In fact, IM Midazolam as the first drug of choice, is perhaps the best option and has been found superior to other drugs, for reasons, which include:
- It is superior to other medications that are not given intravenously(10)
- It gives the most rapid control, probably secondary to minimal time wastage trying to obtain IV access(11)
- It can, if needed in adults, be given via intranasal and buccal routes at the same dose of 10mg.
In a review of 19 studies comparing IM midazolam and rectal diazepam in seizures(12), they found:
- No real difference between time of drug administration and clinical seizure cessation.
- Buccal midazolam may be more effective than rectal diazepam
Dosage:
- In adults and children: IV/IM/IO 0.15mg/kg
- In children:
- Buccal: 0.3mg/kg to a maximum of 10mg
- Intranasal: 0.2-0.5mg to a maximum of 10mg
Second Line Treatment
Benzodiazepines are used as the first line treatment and although some authors propose the use of benzodiazepine infusions as second line agents, their resultant hypotension and respiratory depression has seen a move towards anti-epileptic agents. There is a choice of anti-epileptics to use, which include Phenytoin, Valproic Acid and Levetiracetam.
The aim of second line treatment is to establish a therapeutic level of anti-epileptic. It is reasonable that if the patient is already on an anti-epileptic, to give an IV dose of the same.
In a meta-analysis on anti-epileptic agents, it was found that valproic acid controlled seizures in 75% of cases, levetiracetam in 68% of cases and phenytoin in 50% of cases (13). The data is conflicting and other studies have shown no differences between these three medications(14). There is a scarcity of randomised clinical trials that look at which anti-epileptic is the best to use. In past guidelines the use of phenytoin was favoured, however newer guidelines (15) look at possible options given above.
The ESETT Trial( Established Status Epilepticus Treatment Trial), is underway at present and will compare, in the largest blinded study to date, the efficacy of Phenytoin, Valproic acid and Levetiracetam.
PHENYTOIN
It is perhaps the most popular of the anti-epileptics as it the one drug we are most familiar with. It is a Sodium Channel Blocker and cytochrome P450 inducer. It does have a side effect profile which includes hypotension and bradycardia, including atrial-ventricular blocks. It may not be as effective as Valproic Acid in those with a past medical history of primary generalised epilepsy.
Dosage
15-20 mg/kg given at 50mg/min. This is a total in a 70kg male of 1-1.4g.
Adults: give 1g over 30 minutes
VALPROIC ACID
Causes Na channel inactivation and inhibits cytochrome p450. It can cause hepatotoxicity and thrombocyte dysfunction.
Dosage
20-40mg/kg IV over 10 minutes. A further dose of 20mg/kg can be given over 5 minutes, if still seizing.
For a 70 kg male 20 x 70 = 1.4g, 40 x 70 =2.8g. give 2g over 10 minutes.
Maximum dose is 3g.
LEVETIRACETAM
This appears to be a safe drug, with minimal drug interactions, and no side effect profile. Plus it can be given quickly and works quickly. It does accumulate in patients with renal dysfunction.
Dosage
1g-4g IV over 15 minutes, or 2g over 5 minutes and can repeat.
Third Line Treatment: Refractory Status Epilepticus
Seizures that persist past second line management are described as refractory. At this stage anaesthetic agents are recommended and the induction of a therapeutic coma. There is no evidence that this improves mortality. In most cases at this point, if the patient has not already been intubated, they will need their airway secured.
The three medications normally considered here include, Midazolam, Propofol and Thiopental. Ketamine is considered a fourth line agent. There are no good studies looking at which medication to use and such we will consider the most popular and readily available.
PROPOFOL
It has a rapid onset and is a rapidly cleared drug, mostly by hepatic glucoronidation. It can cause hypotension as its main side effect.
Dosage
2-5mg/kg IV
KETAMINE
It is an NMDA receptor antagonist, with a rapid onset and is metabolised by cytochrome p450. It causes a dissociative state normally.
How does Ketamine work in seizures when it is so very different to the other drugs?
Phenytoin and Benzodiazepines are g-aminobutyric acid (GABA) ergic agents, whereas Ketamine works as a N-methyl-D-aspartate (NMDA) antagonist. GABA receptors exert an inhibitory influence to excitation
As a seizure continues GABA receptors are internalised via endocytosis, resulting in a lack of inhibitory control. This makes GABA ergic agents ineffective. At the same time, the number of excitatory NMDA receptors increases and their stimulation by Glutamate may propagate seizures(16)(17).
Usually Ketamine is used as the fourth anaesthetic agent. Its ability to terminate seizures has been reported as around 30%(18) in some studies and as high as 60% in others. It is believed that earlier use of the drug can result in a greater efficacy(19).
Dosage
Generally a dose of 1–2 mg/ kg, followed by maintenance at an infusion rate of 1-2 mg/kg/h has resulted in high success rates.
Paediatric doses that have been recommended are 2–3 mg/ kg bolus of ketamine every 5 min for a total of 2 administrations, followed by maintenance at a rate of 10– 60 mg/kg/min) for several days.
Super Refractory Status Epilepticus
Up to 10% of patients who present in status epilepticus, proceed to develop super refractory status epilepticus(18). This tends to occur in those with a traumatic brain injury and in NORSE(new-onset refractory status epilepticus, usually in you patients with no history of epilepsy(20).
In this group of patients infusions of both Ketamine and Propofol have been found to be effective(21).
MY APPROACH
When a patient presents with seizures, The approach is:
- All early stabilisation
- Resus cubicle
- oxygenation
- Focussed Examination
- Give MIDAZOLAM 10mg IM, or 0.15mg IV and repeat half dose
- Quick History including any history of seizures
- If seizure stops within 5 minutes load with anti-epileptic, if not, load and prepare to intubate
- Anti-epileptic of choice is Levericatem 2g IV over 15 minutes and a further 2g over 5 minutes
- Propofol(1-2mg/kg IV) and Ketamine (1-2mg/kg IV) plus suxamethonium, for intubation
- If still seizing continue propofol as infusion +/- Ketamine
References
- DeLorenzoRJ,HauserWA,TowneAR,BoggsJG,PellockJM,PenberthyL,etal.A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology 1996;46:1029–35.
- HockerS,TatumWO,LaRocheS,FreemanWD.Refractoryandsuper-refractory status epilepticus—an update. Curr Neurol Neurosci Rep 2014;14:452.
- Kramer U, Chi CS, Lin KL, Specchio N, Sahin M, Olson H, et al. Febrile infection- related epilepsy syndrome (FIRES): pathogenesis, treatment, and outcome: a multicenter study on 77 children. Epilepsia 2011;52:1956–65.
- Jenssen S, Gracely EJ, Sperling MR. How long do most seizures last? A systematic comparison of seizures recorded in the epi- lepsy monitoring unit. Epilepsia. 2006;47(9):1499–503.
- Hunter G, Young B. Status epilepticus: a review, with emphasis on refractory cases. Can J Neurol Sci 2012;39:157–69.
- BrophyGM,BellR,ClaassenJ,AlldredgeB,BleckTP,GlauserT,etal.Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 2012;17:3–23.
- Chen JWY, Wasterlain CG. Status epilepticus: pathophysiology and management in adults. Lancet Neurol. 2006;5(3):246–56.
-
Gaetano Zaccaraa, Gianfranco Giannasib, Roberto Oggionic, Eleonora Rosatid,Luciana Tramacerea, Pasquale Palumbod, on behalf of the convulsive status epilepticus study group of the uslcentro Toscana, Italy. Challenges in the treatment of convulsive status epilepticus. Seizure 47 (2017) 17–24
- Deeb TZ, Maguire J, Moss SJ. Possible alterations in GABAA receptor signaling that underlie benzodiazepine-resistant seizures. Epilepsia 2012;53(Suppl. 9):79–88.
- Dingledine R, Borges K, Bowie D, Traynelis SF. The glutamate receptor ion channels. Pharmacol Rev 1999;51:7–61.
- Arya R, Kothari H, Zhang Z, Han B, Horn PS, Glauser TA. Efficacy of nonvenous medications for acute convulsive seizures: a network meta-analysis. Neurology 2015;85:1859–68.
-
Silbergleit R, Durkalski V, Lowenstein D, Conwit R, Pancioli A, Palesch Y, et al. Intramuscular versus intravenous therapy for prehospital status epilepticus. NEngl J Med 2012;366:591–600.
-
Yasiry Z, Shorvon S. The relative effectiveness of five antiepileptic drugs in treatment of benzodiazepine-resistant convulsive status epilepticus: a meta- analysis of published studies. Seizure 2014;23:167–74.
-
Mundlamuri RC, Sinha S, Subbakrishna DK, Prathyusha PV, Nagappa M, Bindu PS, et al. Management of generalised convulsive status epilepticus (SE): a prospective randomised controlled study of combined treatment with intravenous lorazepam with either phenytoin, sodium valproate or levetir- acetam – Pilot study. Epilepsy Res 2015;114:52–8.
-
Brophy, G.M.; Bell, R.; Classen, J.; Alldredge, B.; Bleck, T.P.; Glauser, T.; LaRoche, S.M.; Riviello, J.J., Jr.; Shutter, L.; Sperline, M.R.; et al. Guidelines for the Evaluation and Management of Status Epilepticus. Neurocritical Care Society Status Epilepticus Guideline Wiriting Committee. Neurocrit. Care 2012, 17, 3–23.
- Holtkamp M, Othman J, Buchheim K, Masuhr F, Schielke E, Meierkord H. A “malignant” variant of status epilepticus. Arch Neurol. 2005;62:1428–31.
-
Gaspard N, Foreman B, Judd LM, Brenton JN, Nathan BR, McCoy BM, et al. Intravenous ketamine for the treatment of refractory status epilepticus: a retrospective multicenter study. Epilepsia 2013;54:1498–503.
-
Redecker J, Wittstock M, Benecke R, Rösche J. Comparison of the effectiveness of four antiepileptic drugs in the treatment of status epilepticus according to four different efficacy criteria. Epilepsy Behav 2015;49:351–3.
-
Ferlisi M, Shorvon S. The outcome of therapies in refractory and super- refractory convulsive status epilepticus and recommendations for therapy. Brain 2012;135:2314–28.
-
Rathakrishnan R, Wilder-Smith EP. New onset refractory status epilepticus (NORSE). J Neurol Sci 2009;284:220.
-
Sabharwal V, Ramsay E, Martinez R, Shumate R, Khan F, Dave H, et al. Propofol- ketamine combination therapy for effective control of super-refractory status epilepticus. Epilepsy Behav 2015;52:264–6.




