THE CASE
A 75 yo man is brought into your small rural ED after 3 hours of ischemic chest discomfort. His background is significant for hypertension, a CVA 5 years ago for which he is on aspirin/dipyrimidole, and 2 coronary artery stents in 1995. The ambulance officers found the patient to be in AF, with a ventricular rate of 170/min, and have given aspirin only. The patient denies any knowledge of any other cardiac history (apart from the stents), and there is nothing in his medication list for rate control, or anticoagulation. He is not aware of palpitations
His initial vital signs are HR 170, BP 108/73, RR 22, SpO2 98% RA, T 36.8. Physical examination shows a moderately elevated JVP, with an otherwise normal examination with no focal neurology, no other signs of heart failure, and no murmurs.
His initial bedside venous bloods show pH 7.39, CO2 38, HCO3 23, K 5.5, Na 142, creat 98. His initial Tn is 0.02
His initial ECG is shown below:
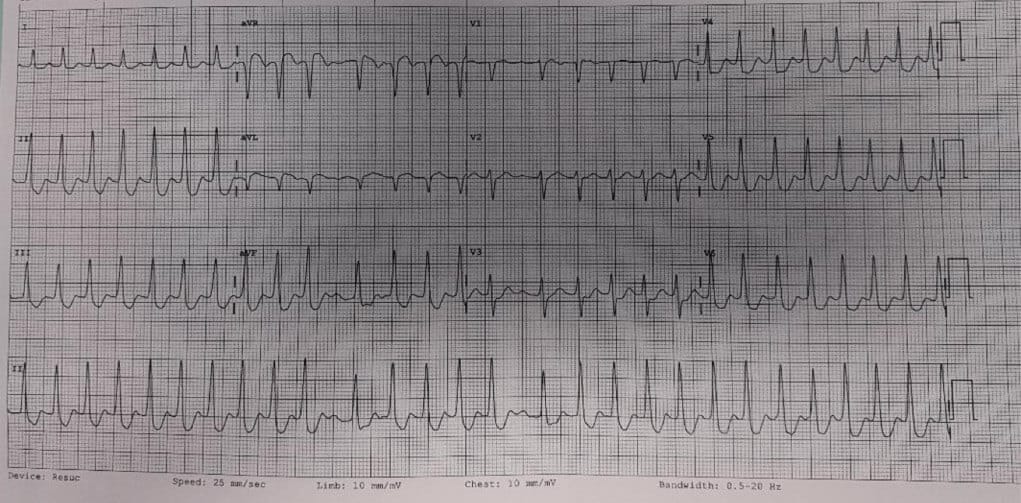
The question in my mind: Is this patient having ischaemia from his AF, or having AF from a primary ischaemic event?
What do you do?
There are 2 major learning points from this case – the management of the unstable AF patient, and the management of this ischaemic ECG pattern (ST elevation in aVR and widespread ST depression)
THE UNSTABLE AF PATIENT
First, how do we define instability in AF? Principally, it’s hypotension, heart failure, or acute ischaemia. And secondly, what do we do about it?
MANAGEMENT OF UNSTABLE PATIENTS IN AF
Most guidelines advocate immediate cardioversion of these patients. However, this is not without its risks. Cardioversion carries with it the risk of embolic complications (especially in patients with elevated risk of stroke, most commonly estimated with the CHA2DS-2Vasc score), and in those who have been in AF for > 48 hours. Also, as most of these patients require sedation for cardioversion, sedation in unstable patients carries with it an elevated risk.
There are 2 principles to keep in mind here
PRINCIPLE # 1 – AF is rarely the cause of instability in ED patients. Most commonly, it is due to sepsis, bleeding, PE, toxic causes etc and the AF is a secondary issue.
In unstable ED patients with AF, a rapid but thorough search for other underlying causes of instability must be conducted, and any underlying cause treated aggressively.
PRINCIPLE # 2 – Not all patients who are unstable require IMMEDIATE cardioversion. A more nuanced assessment will identify that a patient with a systolic BP of 90 but who is mentating well without overt ischaemia or heart failure has a little more time for us to address the instability than a patient who has end organ hypoperfusion.
It is worth bearing in mind that one study3 found patients in AF who were unstable with underlying acute medical illness did worse when rate control or rhythm control was attempted.
THE RISK OF STROKE
This also has to be taken into account when deciding to cardiovert patients. For example, a patient with a low risk of stroke, and a clear onset of AF of < 48 hours can be cardioverted much more safely than our patient above, who had a CHA2DS-2Vasc score of 4, and no known onset time. So, a risk benefit analysis needs to take this into account.
IF YOU NEED TO USE RHYTHM CONTROL
DCCV is the technique of choice for the unstable AF patient who needs cardioversion. It is more successful than chemical cardioversion (about 90-97% vs 50-59%), and is faster than chemical cardioversion. This usually requires sedation, and this risks of sedating an unstable patient need to be considered in this risk benefit analysis.
IF YOU DECIDE TO USE RATE CONTROL
Typically we use beta blockers, or non DHB Calcium channel blockers as first line drugs here, usually IV for more rapid onset. Keep in mind that these are negatively inotropic, and so inappropriate in the shocked patient. For patients who have received adequate doses of the first line agent, and who have failed to achieve adequate rate control, digoxin is probably the best second line agent for most patients.
MANAGING THE STROKE RISK
For patients who are cardioverted, the peri cardioversion time brings with it increased risk of stroke, due to dislodgement of thrombus, and from thrombus formation due to atrial stunning. Stroke risk in patients with AF increases with their stroke risk factors (most widely estimated using the CHA2DS2-VASc score), and with the amount of time they have been in AF – the current cutoff for when the stroke risk becomes significantly higher is after being in AF for > 48 hours. Of course, many patients have no clear onset of AF symptoms, and so they should be assumed to have been in AF for > 48 hours. Keep in mind that it doesn’t seem to matter whether patients are electrically or chemically cardioverted, the stroke risk is about the same. While there is some debate in the literature, for most unstable AF patients, if there is no bleeding/contraindication, should be managed with anticoagulation initially, and for most patients with a CHA2DS2-VASc score of > 0, should be continued.
FINALLY, THE STE in aVR ECG
Lots has been written about this ECG pattern occurring in acute coronary syndrome from LMCA occlusion or severe 3 Vessel disease, but it is worth bearing in mind that it can also be seen in diffuse subendocardial ischaemia (post arrest or rate related ischaemia). I said before that it was unclear whether our patient had an acute ischaemic event that put him into AF, or if he went into AF, and his rate caused diffuse subendocardial ischaemia
THE END OF THE CASE
Given our patient was otherwise relatively stable, and that his stroke risk was high, we elected to initially manage him with anticoagulation and rapid rate control. He received enoxaparin, and titrated IV metoprolol. As we did so, his ischaemic symptoms resolved, and his ECG changes showed marked improvement.
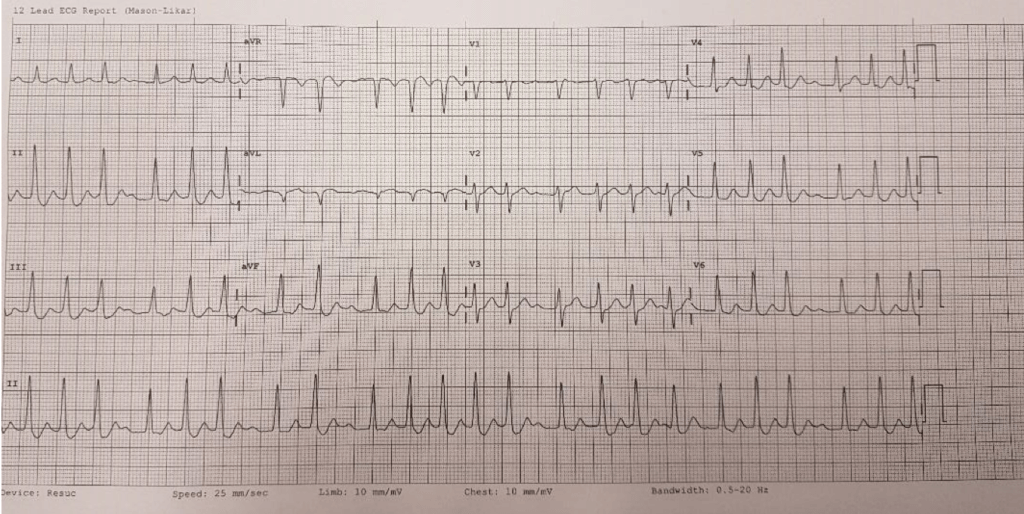
After adequate beta blockade, his rate was still approx. 120 and so he was loaded with digoxin. As his rate settled further, he self reverted to sinus rhythm, and his ECG normalised:
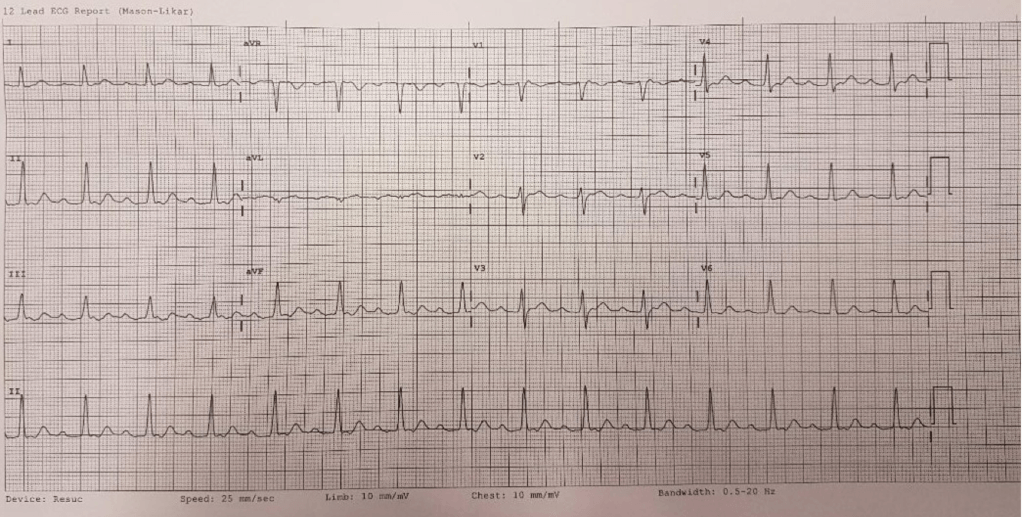
Ultimately the patient did very well and was retrieved to the nearest tertiary centre for cardiac catheterisation.
CONCLUSIONS
Unstable patients with AF are often unstable from another cause. They require a rapid but thorough search for other causes of instability, and aggressive treatment. Not all patients will require immediate cardioversion, however some will. In patients who are relatively stable, pursuing other treatment options can be reasonable, with cardioversion remaining an option for patients who then require it. Patients with AF and ischaemia are a special group, as AF can be either the primary problem or a secondary problem. ST elevation in aVR with widespread ST depression can also be seen in diffuse subendocardial ischaemia, and slowing the heart rate, to improve the supply/demand mismatch can be an appropriate initial strategy for management, especially in centres without timely access to a cath lab. A nuanced approach, individualised to the risks and benefits of the patient in front of you, is the best approach
References
- Atzema, CL and Singh, SM, (2017), ‘Acute Management of Atrial Fibrillation – From Emergency Department to Cardiac Care Unit’, Cardiol Clin 36(1): 141-159.
- Coll-Vinent, B. et al, (2013), ‘Management of acute atrial fibrillation in the emergency department: a systematic review of recent studies’, Eur J Emerg Med 20:151-159.
- Scheuermeyer, FX, et al, (2015), ‘Emergency Department Patients With Atrial Fibrillation or Flutter and an Acute Underlying Medical Illness May Not Benefit From Attempts to Control Rate or Rhythm’, Ann Emerg Med. 65(5):511-522.
- Cohn, BG, et al, (2013), ‘Is Emergency Department Cardioversion of Recent Onset Atrial Fibrillation Safe and Effective?’, J Emerg Med. 45:1: 117-127.
- Russo, V. et al, (2013) ‘Management of atrial fibrillation in the Emergency Department: current approach and future expectations’, Eur Rev Med Pharmacol Sci. 17: 3132-3147.
 Dr Adam Michael
Dr Adam Michael



