Differentiating between Pericarditis, Benign Early Depolarisation and ST Elevation Myocardial Infarction can sometimes be difficult.
CASE
A 35 yo male presents with palpitations and pleuritic chest pain. He’s recently had a viral illness but has no other medical history. At 1am in the morning, the patient was woken by palpitations. He now complains of left sided chest pain and dyspnoea. His vitals are normal.
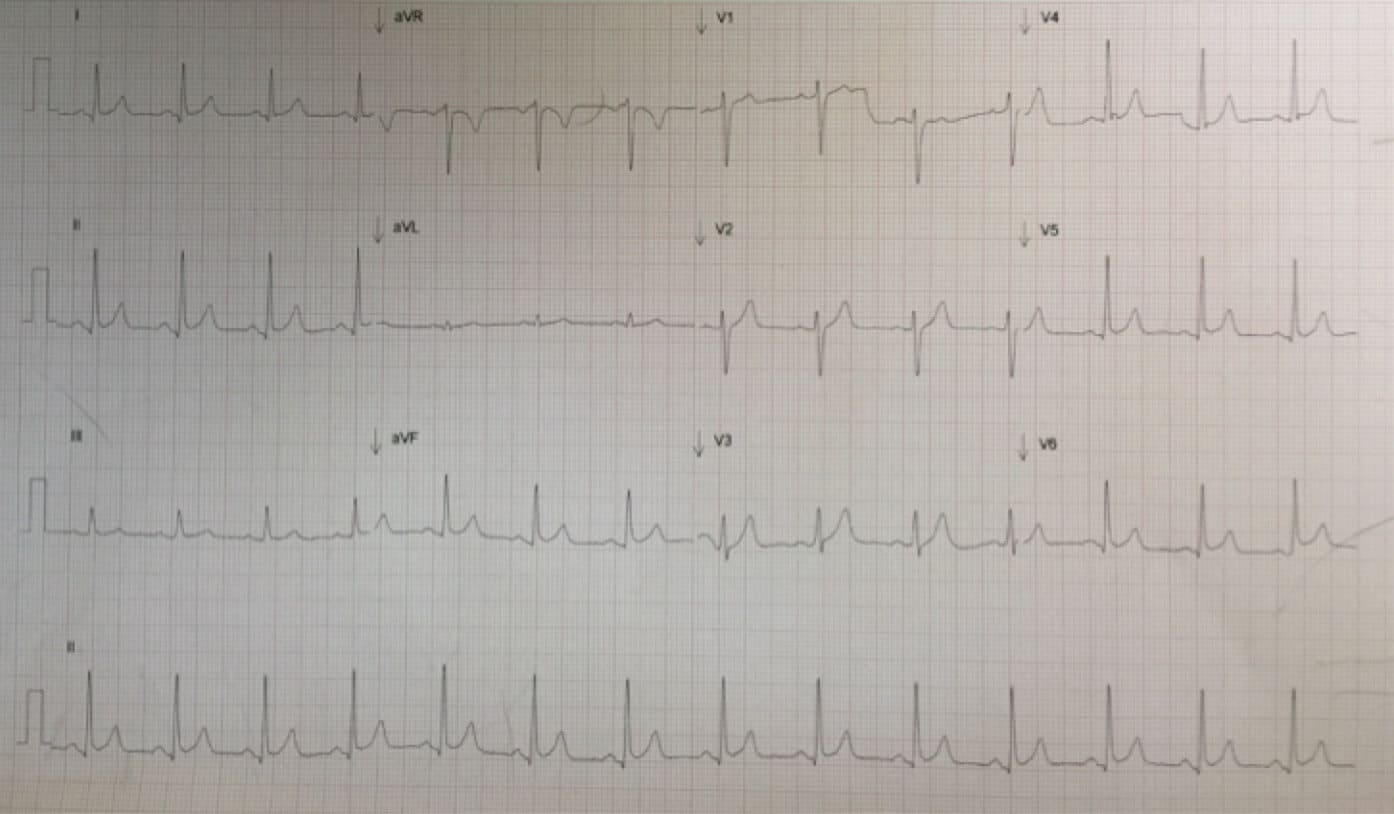
His ECG is shown below:
 What is the diagnosis?
What is the diagnosis?
Is this a pericarditis, or Benign Early Repolarisation(BER) or ST elevation myocardial Infarction(STEMI)?
HOW DO WE DIAGNOSE PERICARDITIS?
A December 2014 NEJM article(1) provides a good clinical practice review of this topic.
To diagnose pericarditis we need a minimum of 2 of the following 4 criteria:
1 Typical chest pain
-Especially pleuritic pain, preacordial or retrosternal, relieved by sitting forward
-Pain that radiates to trapezius ridge(2) (considered pathognomonic)
2 Pericardial Friction Rub– this is transient
3 Typical ECG changes
-ST elevation across several territories
-PR depression
– No reciprocal ST depression, except in aVR + V1
4 Pericardial effusion
-Usually described as > 20mm in width
If we analyse this ECG using the ECG in 20 seconds approach:
Rate: 84 bpm
P waves: Upright in I, II and inverted in aVR = leads in right place and normal sinus rhythm
QRS: Not too tall, not too small, normal morphology and no clumping
ST-T segments Saddle shaped elevation in II, avF, V4-6 – this widespread ST elevation with no reciprocal changes ie., no reciprocal ST depression, indicates pericarditis.
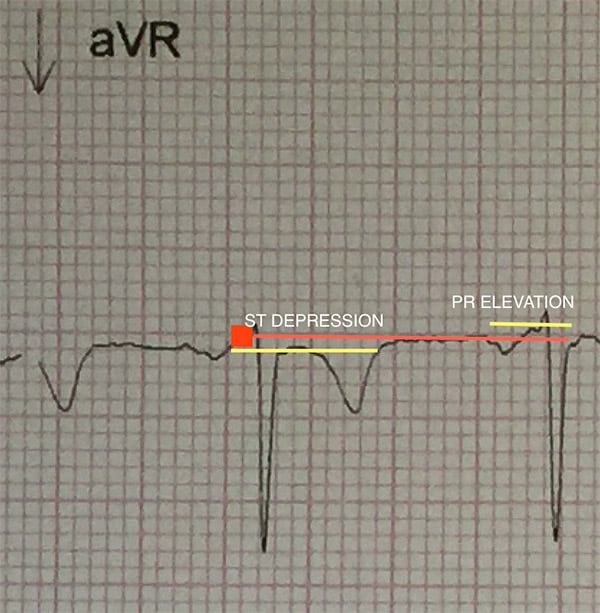 There is ST depression in aVR as well as PR elevation- This indicates pericarditis.
There is ST depression in aVR as well as PR elevation- This indicates pericarditis.
Intervals: PR and QT are normal, but there is PR depression in some leads
What other features do we see in this ECG?
1 There is J-point notching in V4 which is more consistent with BER.
2 The ST Segment/T wave ratio is ¼ = 0.25- this doesn’t help us as >0.25 = pericarditis.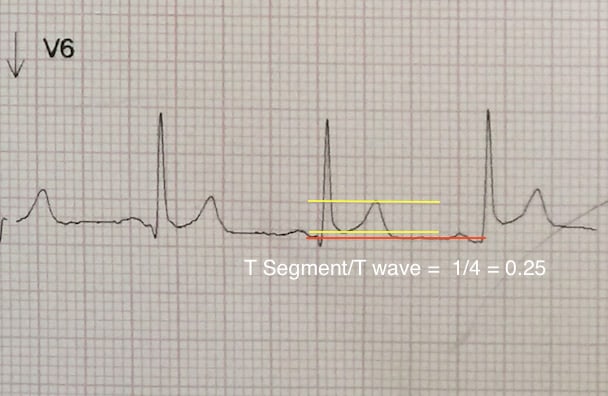
My diagnosis in this case is that this is probably acute pericarditis on the background of BER.
How to differentiate Pericarditis from Benign Early Repolarisation (BER)?
Requirements for pericarditis
-T waves normal, non prominent
-No fish hook, ie., J point, especially in V4
-Spodick’s Sign: There is a downslope of the ST-T segment.
-ST segment elevation/T wave is >0.25 in pericarditis
Differentiating STEMI from Pericarditis or BER?
-If there is ST depression in any other lead except aVR, it is iscahemia.
-ST elevation III>II is a STEMI
-QR-T Sign occurs in STEMI
So what do we do with this patient?
His clinical presentation points to a pericarditis. There are changes in his ECG that support that, however there are also changes that support BER. However there is no evidence of a STEMI.
-My approach is to treat him as a pericarditis. Patients with BER may also have pericarditis.
What causes pericarditis?
Viral infections are the main cause, however they may also be due to bacteria and tuberculosis. It can be due to immune causes such as SLE.
It can also be caused by trauma, medications and patient may present post MI. This patient volunteered that he had a recent viral illness, which helps us with the diagnosis.
Any other investigations to do?
Labs
1 Troponin- in case this is myopericarditis
2 CRP- this gives an indication of the progress of the disease and may be helpful if admitted
Radiology
1 CXR- may show a widened mediastinum and alert you to a pericardial effusion
2 ECHO – we can do a bedside echo looking for a significant pericardial effusion. What is significant is described as being >20mm in width. These are only present in about 3% of patients(3). If a patient is going home they probably can also have a more formal outpatient ECHO.
What is the treatment of Pericarditis?
1 NSAIDS 600-800mg 6-8/24 or Aspirin 2-4g daily in divided doses. Continue for 1 week
2 Colchicine 0.5mg bd if >70kg and 0.5mg daily if <70kg. Continue for 3 months(4)
I would also add a proton pump inhibitor.
What about steroids as the anti-inflammatory agent of choice. There is evidence to say that it results in a greater rate of recurrence(3).
Who can we send home?
The presence of any of these 5 factors that determine the need for admission:
-Fever > 38o C;
-Subacute onset;
-Large pericardial effusion;
-Cardiac tamponade; and
-Lack of response to aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) after at least 1 week of therapy.
References
1 LeWinter M.M. Acute Pericarditis. NEJM 371;25, Dec 18 2014 pp 2410-2416
2 Maisch B et al. Guidelines on the diagnosis and management of pericardial diseases executive summary. Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Eur Heart J 2004;25:587-610
3 Imazio M et al. Treatment with aspirin, NSAID, corticosteroids and colchicine, in acute and recurrent pericarditis. Heart Fail Rev 2013;18;355-360
4 Imazio M et al. A randomised trial of colchicine for acute pericarditis. NEJM 2013;369:1522-1528
Peter Kas



